Uganda Zero-Dose Landscape

Background
The Gavi Zero-Dose Learning Hub (ZDLH) is responsible for highlighting work and outputs generated by the four Gavi Country Learning Hubs (CLHs) in Bangladesh, Mali, Nigeria, and Uganda with the objective of using this evidence to better understand the factors influencing implementation and performance of approaches to identify and reach zero-dose (ZD) and under-immunized children as well as missed communities. The consortium is led by JSI Research & Training Institute, Inc. (JSI) in partnership with the International Institute of Health Management Research (IIHMR) and The Geneva Learning Foundation (TGLF). Together, the group aims to support CLHs to implement Gavi's Identification-Reach-Monitoring-Measurement-Advocacy (IRMMA) framework; facilitate sharing and learning across the CLHs; contribute evidence to capture, synthesize, and disseminate the breadth of learning across the Gavi Alliance; and ultimately help improve immunization equity and reduce the number of ZD and under-immunized children globally by facilitating quality evidence generation and uptake.
In pursuit of these objectives, the ZDLH has developed ZD landscapes to synthesize the evidence to date on immunization prevalence, policy, and programming in each of the four learning hub countries. These landscapes describe the current immunization and ZD context, including coverage trends, equity, health systems, and existing partners and programming to orient implementers and funders to the broad immunization context and opportunity for intervention to reduce the prevalence of ZD children. While these landscapes present the findings of syntheses of existing literature, the CLHs in Uganda and other countries will generate evidence based on their own country-level ZD programming and activities such as rapid assessments and surveys.
The purpose of this landscape is to provide the Gavi CLH and stakeholders in Uganda with a comprehensive overview of the immunization landscape within the country, with a special focus on ZD and under-immunized children. Gavi defines a ZD child as one who has not received a single dose of a diphtheria, tetanus, and pertussis-containing vaccine. Given the highly variable and contextual nature of the drivers, barriers, and programmatic approaches to reach ZD and under-immunized children, it is important to understand the unique context, policies, and economics of the country to help guide approaches, but also to better understand and interpret why changes in IRMMA may or may not occur. This landscape also aims to inform research and programming efforts in Uganda by identifying important knowledge gaps that pertain to the IRMMA framework for ZD and under-immunized children.
Methods
The ZD landscape assessments are based on literature reviews and secondary data analyses. To identify relevant literature, the ZDLH team searched both gray and peer-reviewed sources, ministry and partner websites, and Gavi reviews and resources. Domains of interest include immunization coverage and equity and information about the health system in which the immunization program operates including but not limited to human resources, financing, immunization policies, and the health system structure. Relevant publications are identified and reviewed and information related to the ZD or immunization context in each country is extracted. Where gaps in information remain, the team relies on input from members of the CLH and key informant interviews (KIIs) conducted as part of the complementary political economy analysis (PEA). These landscape analyses are intended to represent the current situation in the countries and will be updated annually to include new resources including those generated by the CLHs.
Introduction
The delivery of vaccines that protect against preventable childhood diseases has been Uganda’s health system priority for several decades and has resulted in significant improvements in vaccination coverage and child mortality rates. The number of children who have received all basic vaccinations has increased approximately 20 percent since 2001.1 Additionally, mortality among children under five has decreased nearly 71 percent since 2000.2 Despite this progress, just over half of Ugandan children ages 12–23 months have received all basic vaccinations.3 Challenges in coverage and equity persist and coverage rates vary greatly from region to region. Children in urban slums and areas that are rural, hard-to-reach, and home to refugee populations are more likely to be under- and un-immunized. Identifying approaches to track and reach these children is critical to meeting the goal of full and equitable immunization coverage in Uganda.
Uganda is a landlocked country in East Africa that lies along the equator and shares borders with five countries (Figure 1). As of 2022, it had 47,249,585 people, of whom 7,868,838 are children under five (Table 1).4
Figure 1. Map of Uganda
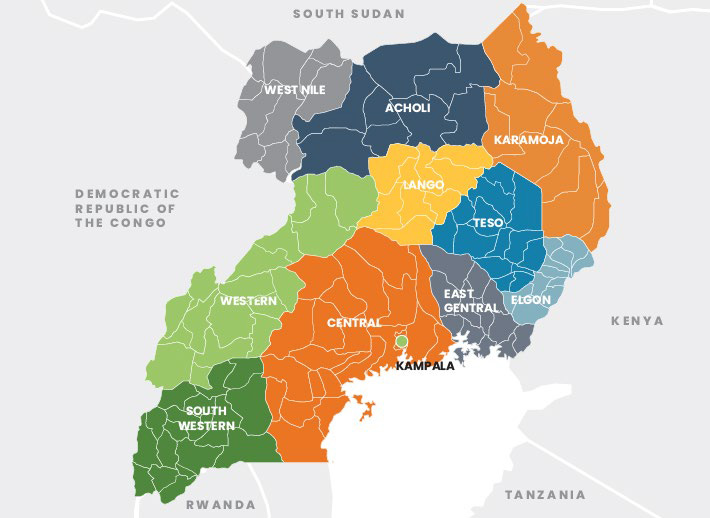
Table 1. Total Population and Residence
| Total Population (2022) | |
|---|---|
| Total | 47,249,585 |
| Male | 23,401,332 (49.5%) |
| Female | 23,848,254 (50.5%) |
| Residence (2022) | |
|---|---|
| Rural | 73.8% |
| Urban | 26.2% |
Source: United Nations, Department of Economic and Social Affairs, Population Division. World Population Prospects, 2023.
Although Uganda has achieved a 71 percent decrease in mortality among children under five since 2000 (Figure 2), the United Nations Inter-agency Group for Child Mortality Estimation (UN-IGME) estimates that in 2021, approximately 69,000 children under five died from a variety of causes including vaccine-preventable diseases.
Source: United Nations Inter-agency Group for Child Mortality Estimation (2023).
The 2019 Global Burden of Disease study found that approximately 20 percent of deaths among children under five in Uganda were caused by illness that may have been vaccine-preventable, including measles, meningitis, whooping cough, and some lower-respiratory infections (Figure 3).
Source: Institute for Health Metrics and Evaluation (IHME). GBD Results, Uganda. Seattle, WA: IHME, University of Washington, 2020.
Improved access to immunization is a principal driver of the decrease in under-five mortality in developing countries.5 Three decades of routine immunization programs have contributed to declines in vaccine-preventable diseases such as measles in countries like Uganda (Figure 4).
Source: IHME. GBD Results, Uganda. Seattle, WA: IHME, University of Washington, 2020. (Accessed June 29 2023); ICF, 2015. The DHS Program STATcompiler. Funded by USAID. (Accessed June 29 2023).
Immunization Context
Despite increases in vaccination coverage over time, gaps in immunization continue to contribute to under-five morbidity and mortality in Uganda. Households that include children who have not received a single dose of the pentavalent (penta) vaccine series are estimated by a recent Gavi analysis to represent 13 percent of the 10,847 deaths among children under five in the country.6
Immunization Schedule
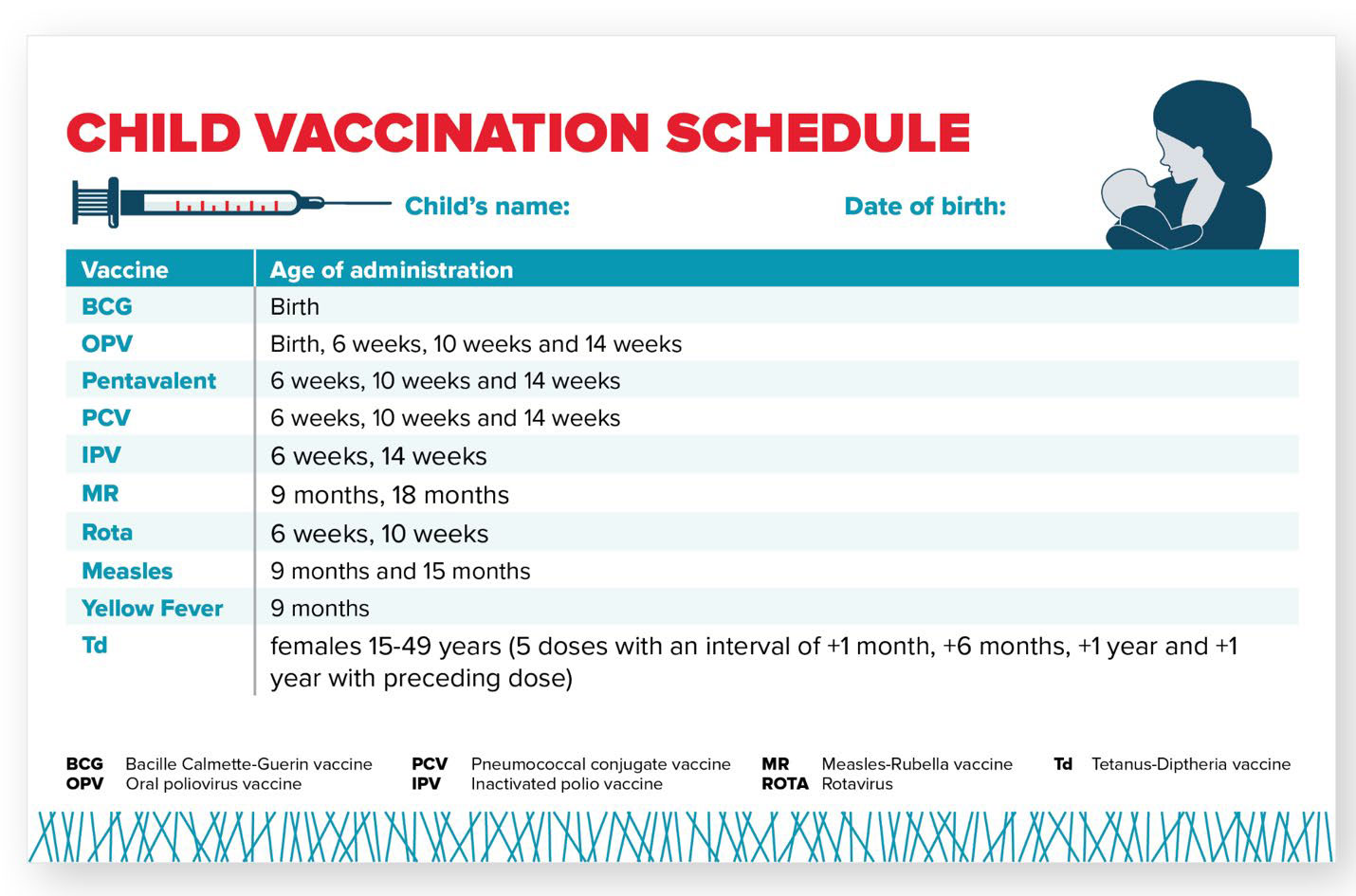
Uganda’s immunization schedule includes nine different vaccines and targets approximately two million children each year. Uganda administers the penta vaccine, which protects against diphtheria, tetanus, pertussis, hepatitis B, and Haemophilus influenzae type b (Hib) (Figure 5).
Figure 5. Uganda Childhood Vaccination Schedule
Coverage Estimates
Current coverage estimates for six basic immunizations in Uganda range from 94 percent of children receiving Penta1 to 49 percent receiving the second dose of the measles-containing vaccine (MCV) (Figure 6). Uganda could prevent an estimated 513,800 future deaths through currently forecasted preventive immunization activities between 2021–2025.7
Source: World Health Organization/UNICEF Estimates of National Immunization Coverage (WUENIC)—2022 estimates. (2022). WHO Immunization Data Portal.
Identifying and reaching ZD and under-immunized children in Uganda is essential to meet the Gavi 5.0 equity goal and to progress toward reaching all eligible children with routine vaccination in the country.
Estimating the number of ZD children in Uganda requires estimates of Penta1 coverage and the total number of surviving children. These estimates can vary based on the source of the data resulting in different estimates of the ZD population (Table 2). Positive estimates (those above zero) range from 100,096 (from the WHO/UNICEF Estimates of National Immunization Coverage [WUENIC]) to 131,328 ZD children (Institute for Health Metrics and Evaluation [IHME]).8
Table 2. Uganda ZD Estimate Inputs
| Source | Total Number of Surviving Infants | Penta1 Coverage | Number of ZD Children |
|---|---|---|---|
| WUENIC (2022) | 1,668,269 | 94% | 100,096 |
| IHME (2021) | 1,641,604 | 92% | 131,328 |
Source: Gavi Secretariat. 2022. “Uganda Zero Dose Analysis.” Unpublished. World Health Organization/UNICEF Estimates of National Immunization Coverage (WUENIC)—2022 estimates. (2022). WHO Immunization Data Portal.
Uganda’s national administrative data from 2021 estimate Penta1 coverage at 97 percent. At the subnational level, however, 51 of 136 districts estimated coverage to be over 100 percent. Coverage rates of over 100 percent may indicate an error in the documentation of the number of children receiving Penta1 vaccines or in estimates of the total number of children.9
The goal of WUENIC analyses is to provide national immunization estimates on an annual basis. WUENIC immunization estimates are developed by triangulating data from several sources including government data, published and unpublished survey data, and consultation with local experts and governments. Statistical and mathematical modeling are not used to derive the final coverage estimates and estimates are not available at the sub-national level. As such, WUENIC estimates are not useful for identifying the location of ZD children in the country, but are useful for looking at trends in the ZD population over time.
IHME projections include different inputs and analyses because the goal of these estimates is different from those of WUENIC or administrative data. The goal of IHME is to generate highly-specific geospatial estimates of immunization coverage that are combined with additional data to generate national coverage estimates. IHME, like WUENIC, uses household survey data as well as national data, but it also uses covariates of immunization (such as residence or mother’s level of education) when calculating estimates. Using this data, IHME models immunization coverage at a hyper-local level (a five-by-five kilometer [km] area) and then incorporates additional higher-level data to model a national estimate.10 The resulting estimates provide more insight into the probable locations of ZD children within a country, but also include more assumptions and potential error than estimates generated from household surveys or administrative data.
Given the differences in source data and estimation approaches, the true number (and location) of ZD children is not known. However, by triangulating the various estimates, we can determine where there is overlap and generate an informed best guess that can be used for broad planning purposes. Tailored implementation strategies to vaccinate ZD children may require other methods to better understand where they are located, how to reach them and how to effectively bring them into routine immunization services.
For the purposes of this landscape, we will use data from both WUENIC and IHME sources, with the understanding that the estimates are imperfect. Data from household surveys like the Uganda Demographic and Health Surveys (DHS), will also be incorporated into this assessment, particularly for equity analyses.
Effects of the COVID-19 Pandemic
Uganda reported its first case of COVID-19 on March 21, 2020, leading to nationwide mitigation measures including non-essential travel restrictions, discontinuation of public transportation, bans on group gatherings, and school and workplace closures. Lockdown measures were lifted in phases starting in mid-May 2020. By March 2021, the country’s activities had largely resumed to pre-pandemic levels, but schools remained closed until January 2022.11 Uganda’s rapid and comprehensive response to COVID-19 during its first and second waves minimized early morbidity and mortality.12 However, mitigation measures disrupted maternal and child health services, including immunization. A study of COVID-19’s impact on maternal, newborn, and child health (MNCH) services in Kampala found that while immunization clinics were considered “essential” and run according to pre-pandemic schedules for the duration 2020, there was a decrease in average monthly attendance.13 A separate study of caregivers and other key informants in Kampala and Wakiso revealed that access to and lack of funds for transportation and fear of contracting COVID-19 were the main barriers to accessing immunization services during the first two waves of the pandemic.14
WHO and UNICEF estimate that diphtheria, tetanus, and pertussis 3 (DTP3) coverage in Uganda fell from 93 percent pre-pandemic to 89 percent in 2020.15 However, efforts from the government alongside partners brought coverage rates up to 91 percent by 2021. Additionally, DTP1 coverage rose to 97 percent in 2021 from 96 percent in 2019.16 Uganda’s Expanded Programme on Immunisation (EPI), anticipating the pandemic’s disruption to routine immunization services, ordered stockpiles of routine vaccines before international travel was disrupted, effectively avoiding stockouts. Additionally, the Ugandan Ministry of Health (MOH) and the Clinton Health Access Initiative (CHAI) developed guidelines to integrate COVID-19 services with other health services, including routine immunization. Reviews of health facility immunization registration data enabled the country to identify underserved areas, leading to a 50 percent increase in the number of children in those areas vaccinated against DTP3 and measles and rubella 1.17
Equity
Gavi’s 5.0 strategy to identify and reach ZD and under-immunized children focuses on equity. To comprehensively implement Gavi’s 5.0 strategy, it is essential to examine the contexts in which ZD and under-immunized children live.
Factors Influencing ZD Status
Figure 7 presents sociodemographic characteristics for children who did not receive the Penta1, Bacillus Calmette-Guérin (BCG), and measles vaccines. These three antigens, given at different times and locations, can represent different immunization access barriers. Penta1 is typically used as a proxy indicator of access to routine immunization because it is given during well-child visits at 6, 10, and 14 weeks.
The measles vaccine, however, is given first at 9 months and again at 18 months old at regional health facilities, which also represents access to routine immunization services, albeit at a later age. BCG is given at birth in Uganda, so its coverage may better represent birth in a health facility than access to routine immunization services.
Source: Uganda Bureau of Statistics - UBOS and ICF. 2018. Uganda Demographic and Health Survey 2016. Kampala, Uganda and Rockville, Maryland, USA: UBOS and ICF.
The data presented in Figure 7 support findings in the literature that indicate that the mother’s education, birth order, and where a child lives are significant predictors of whether or not a child will receive the measles, BCG, or Penta1 vaccine in Uganda. Children of mothers with no or only primary level education are more likely to be ZD than those whose mother received a secondary or higher education. Additionally, children who are the sixth-born or after in their household are more likely to be ZD than those born before them. Finally, a child’s geographic location is an important predictor of ZD status. Among the regions of the country, a greater proportion of ZD children are found in Greater Kampala (7.8 percent) and the east central region (6.9 percent) than in the southwest (2.7 percent) and the mountains (2.1 percent), as indicated in Figure 8. According to IHME estimates, nearly half of ZD children in Uganda live in just 24 percent of districts, which are outlined in black in Figure 8. In addition to disparities in ZD status between geographic locations, there are disparities between ethnic groups. Of the 20 major ethnic groups in the country, the Banyole, at 15.2 percent, has the highest proportion of ZD children, followed by the Batoro, at 8.6 percent). Children in the Bafumbira and Acholi groups are least likely to be ZD, with a prevalence of 0.5 and 0.9 percent, respectively.18 The Banyole group lives primarily in rural areas of Eastern Uganda and largely relies on subsistence farming and small-scale businesses. A 2019 qualitative study of health care access in a district with a majority Banyole population found that a lack of affordable transportation, roads inaccessible to motorized vehicles, and poor service at health facilities were challenges to accessing services.19 Both the Batoro and Bafumbira groups are found in the southwestern region of Uganda, with the Batoro living near Lake Albert and the Bafumbira near the border of Rwanda. The Acholi are located in the northern region of the country.
Figure 8. Number of ZD Children by District
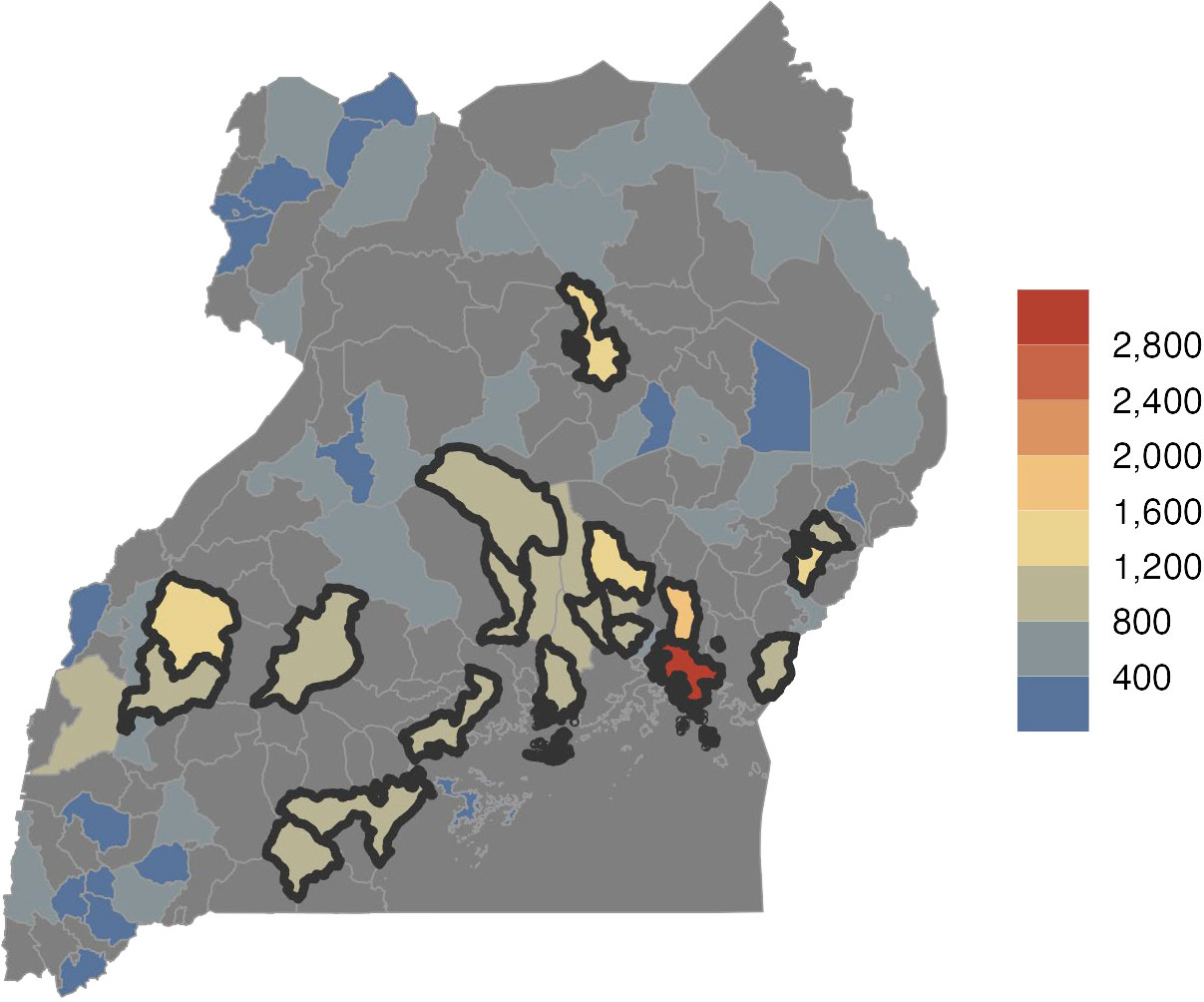
Source: IHME 2021 data cited in Gavi Secretariat, 2023. “Uganda Zero Dose Analysis.” Unpublished.
Despite urban populations being closer to vaccination services, urban areas of the country, particularly Kampala, have a higher proportion of ZD children than less-populated areas.20 According to the country’s most recent census, approximately 60 percent of Kampala’s population live in slum areas.21 Additionally, Kampala hosts a large number of refugees and asylum seekers, the majority of whom come from South Sudan and the Democratic Republic of the Congo.22 A 2022 mixed-methods study of vaccine coverage in Kampala found that inadequate information about the benefits of vaccination, informal fees at vaccination sites, and long wait times to receive services were barriers to immunizing children.23 Additionally, a 2020 evaluation in Kampala found that immunization stock outs and perceived discrimination against refugees and minority groups lessened demand for immunization.24 Results from a descriptive study of the Family Health Days outreach program in 31 districts indicated that caretakers in urban areas are likely to have informal jobs with schedules that are incompatible with immunization service schedules.25
Studies exploring vaccine coverage and hesitancy among the diverse groups living in urban slum settlements, including refugees and ethnic minorities, are largely absent from the literature.
Health Systems
Uganda has a decentralized, referral-based health care system made of the public and private sectors, nongovernmental organizations (NGOs), and donors.26 Figure 9 shows that overall and government spending on health care increased from 26 U.S. dollars (USD) per capita in 2005 to 34 per capita in 2020. Despite this increase, the percentage of gross domestic product spent on health care decreased from 6 percent in 2005 to 4 percent in 2020.27
Source: WHO Global Health Expenditure Database. Health Expenditure Profile, Uganda.
Uganda spends slightly more per capita on health care than most countries in the region (Figure 10).
Source: WHO Global Health Expenditure Database. Health Expenditure Profiles.
However, a better predictor of high immunization coverage is the combination of higher levels of government spending as a proportion of total spending on health care and low out-of-pocket spending.28 These conditions make immunization more accessible to children from the poorest households and their families.29 Out-of-pocket spending as a proportion of total spending in Uganda decreased from 43 percent in 2000 to 37.5 percent in 2020. During that same time period, government spending as a proportion of total spending decreased from 25 percent to 17 percent, with spending remaining relatively stagnant since 2012 (Figure 11). These trends align with those seen in other low-middle income countries.30
Source: World Health Organization. (2022). Global Health Expenditure Database- 2022 Release.
Immunization Financing
Immunization is one of the most important and cost-effective public health interventions. According to one study, for every USD spent on immunization between 2011 and 2020, there was an average return of up to $26 across a child’s lifetime.31 In 2022, Uganda spent approximately 12 million USD on vaccines and routine immunization services, 45 percent of which was financed by the government and 55 percent by external funders.32
Donor Support
Uganda is one of 28 countries in the “initial self-financing” phase of eligibility for Gavi support, making it eligible to apply for new vaccine support or health system and immunization strengthening.33 Gavi is the largest source of external financing for immunization in Uganda, providing more than 27 million USD in immunization programming support, including health systems strengthening funds and new and under-used vaccine support for penta, pneumococcal conjugate, inactivated polio, human papillomavirus, and rotavirus vaccines in 2018 (Figure 12).
Source: Gavi, the Vaccine Alliance Disbursement Data, 2022.
In addition to Gavi, important development partners for immunization in Uganda include the United Nations Children’s Fund (UNICEF), the Clinton Health Access Initiative (CHAI), World Health Organization (WHO), Merck and Company, and the United States Agency for International Development (USAID).34
Ugandan immunization strategies are established primarily by the MOH, which develops policies, mobilizes resources, sets priorities, provides technical support to districts, and convenes stakeholders at all levels of the health system. Each district manages the health facilities under its jurisdiction autonomously and is responsible for planning and managing the delivery of district-level immunization services with the support of national associations and external partners.
The Uganda Virus Research Institute (UVRI) conducts disease surveillance, researches improved vaccination strategies, trains immunologists, and tests vaccine safety and efficacy. It receives funding from the government of Uganda and international organizations such as the WHO and the Bill & Melinda Gates Foundation (BMGF). Other departments that fall under the MOH such as the Department of Integrated Epidemiology, Surveillance and Public Health Emergencies, gather evidence for decision makers.
National Policies
Uganda EPI’s Comprehensive Multi-Year Plan (cMYP) is the main document for outlining immunization-related priorities. The most recent plan was developed for 2016–2020 and outlines achievements since the 2012–2016 plan, including increases in routine vaccination coverage, an increase in the percentage of facilities that report receiving supportive supervision, and the introduction of the pneumococcal conjugate vaccine 10. It also notes remaining immunization-related challenges such as frequent vaccine stock outs, EPI staffing gaps at service delivery sites, and weak coordination between health facilities and community health workers. National objectives set forth in the plan include improving immunization demand; reducing the gap in DTP3 coverage between the highest and lowest socioeconomic quintiles; increasing DTP1 coverage to 98 percent and measles-containing vaccine coverage to 92 percent; and increasing the percentage of districts with detailed immunization microplans to 100 percent. The cMYP prioritizes ZD children as part of its goal to reduce the DTP3 coverage gap but otherwise does not provide a strategy for reaching them.
The inclusion of immunization activities in national strategy and policy documents signals the government’s commitment to reducing vaccine-preventable disease. Table 3 summarizes key government documents that outline immunization activities and targets.
Table 3. National Policy and Strategy Documents Relevant to Immunization
| Policy/Legislation | Year/s | Summary |
|---|---|---|
| Ministry of Health Strategic Plan | 2020/21–2024/25 | This plan has strategies for implementing National Health Policy objectives. It describes the roles and responsibilities of actors across all levels of the health system and includes a roadmap for MOH coordination and communication with stakeholders. |
| Comprehensive Expanded Programme on Immunization Multi-Year Plan | 2016–2020 | The plan guided implementation of vaccine-related activities and set targets and priorities for vaccination, including achieving at least 80% coverage for all routine childhood vaccinations. It also outlined investment decisions and sources of financing for planned activities. |
| Strategy for Improving Health Service Delivery | 2016–2021 | This strategy targets health sector-specific directives identified by the president in 2016. Priorities outlined in the strategy included strengthening human resources for health, scaling up health communication programs with an emphasis on immunization, and establishing supportive supervision guidelines. |
| The Second National Health Policy | 2010 | This policy provided a framework for disease prevention and diagnosis and guided the delivery of the Uganda National Minimum Health Care Package. It included objectives and strategies including strengthening partnerships between the public and private health sectors. |
| First National Health Policy | 1999 | This guided Uganda’s health sector until 2010. Its key objective was to reduce mortality, morbidity, and fertility through 10 implementation strategies, including expanding immunization coverage. |
Human Resources for Health
Adequate human resources are essential for all health care services, including immunization. However, immunization programs require a range of staff, including clinicians, supply chain professionals, logisticians, cold chain technicians, and data enterers. Since 2016, community health extension workers (CHEWs) have been responsible for providing immunization services in Uganda with assistance from village health teams (VHTs) of volunteer community health workers.35 Yet community health workers represent 0.1% of Uganda’s health workforce.36 The WHO National Health Workforce Accounts database indicates that the number of midwifery personnel increased from 2.4 per 10,000 people in 2015 to 5.3 per 10,000 people in 2020. The number of all community health worker cadres, however, decreased from 47.8 per 10,000 people in 2015 to 41.7 in 2020.37 Before 2016, the community health workforce consisted almost exclusively of volunteers who were unable to serve community members consistently.38 CHEWs were introduced in 2016 as a direct and consistent link between the community and health services. In accordance with targets set by the Community Health Extension Workers National Strategy, the total number of community health workers in the country at the end of 2022 included an estimated 15,000 CHEWs (approximately 4 per 10,000 people).39
Analyses of the distribution of community health workers, including CHEWs, between urban and rural communities are largely absent from the literature. Information on the adequacy of CHEW staffing and their effect on immunization and the health care system overall is similarly unavailable.
Health Management Information System Structure and Disaggregation, Data Availability and Use
Uganda’s health management information system (HMIS) was established in 1985. It relied on paper-based data collection at service-delivery sites, and health workers at the community level compiled and summarized data before submitting to higher levels of the system. A 2005 case study found that problems with data timeliness, accuracy, and completeness were due in part to poor data management capacity of staff, unstandardized tools, and inconsistent infrastructure for data management across districts.40
In 2011, after several revisions and expansions, the HMIS evolved into the DHIS2 platform. By 2012, it was deployed to all districts; by 2017, it was available at all levels of the health system.41 A 2014 study of the effect of the DHIS2 on Uganda’s routine health data one year after deployment found that national-level reporting on the proportion of one-year-old children immunized against measles increased from 30 percent in 2011 to 67 percent in 2013. Additionally, the proportion of districts submitting all required outpatient data to the MOH increased from 3 percent to 23 percent during the same time period.42 Given that the DHIS2 had not yet been rolled out to health units below the district level in 2013, there was likely considerable sub-national variation at this time. As of 2021, 97 percent of districts had a reporting rate of at least 90 percent.43
Uganda’s immunization data are collected at health facilities and outreach sites at all levels of the health system. Staff at the service delivery site enter immunization data into a standard reporting form on a mobile phone or computer. The data are forwarded to a district health management team, which merges, aggregates, and sends data to the national level through the DHIS2.44
Uganda’s disease surveillance protocol uses a number of measures to improve HMIS data quality. For example, the DHIS2 system calculates the timeliness and completeness of reports from all reporting sites. Sites that are determined to be low performing are flagged to receive supportive supervision from higher levels. Despite these measures, vaccination data timeliness, completeness, and quality continue to be a concern.45 Findings from a 2017 study indicate that inaccurate immunization data were routinely submitted at the health facility level between 2014 and 2016.46
Comprehensive assessments of immunization data in Uganda were not identified in the literature. Additionally, studies investigating barriers to timely, complete, and high-quality immunization data reporting through the DHIS2 system are gaps in available research in Uganda.
Community Health Structure and Role in Routine Immunization
CHEWs and VHT members are the primary community health providers in Uganda. The structure of Uganda’s community health system and the roles and responsibilities of each cadre are outlined in documents including The Village Health Team Strategy and Operational Guidelines and the Community Health Extension Workers Strategy in Uganda.47 Health center in-charges at the parish/ward levels supervise CHEWs, who supervise VHT members. CHEWs are paid workers who deliver a range of services including vaccination and refer community members to health facility-based services. VHT members are unpaid volunteers who conduct home visits, referrals, community mobilization, immunization advocacy, and some basic MNCH and nutrition services.48
Immunization Program Details
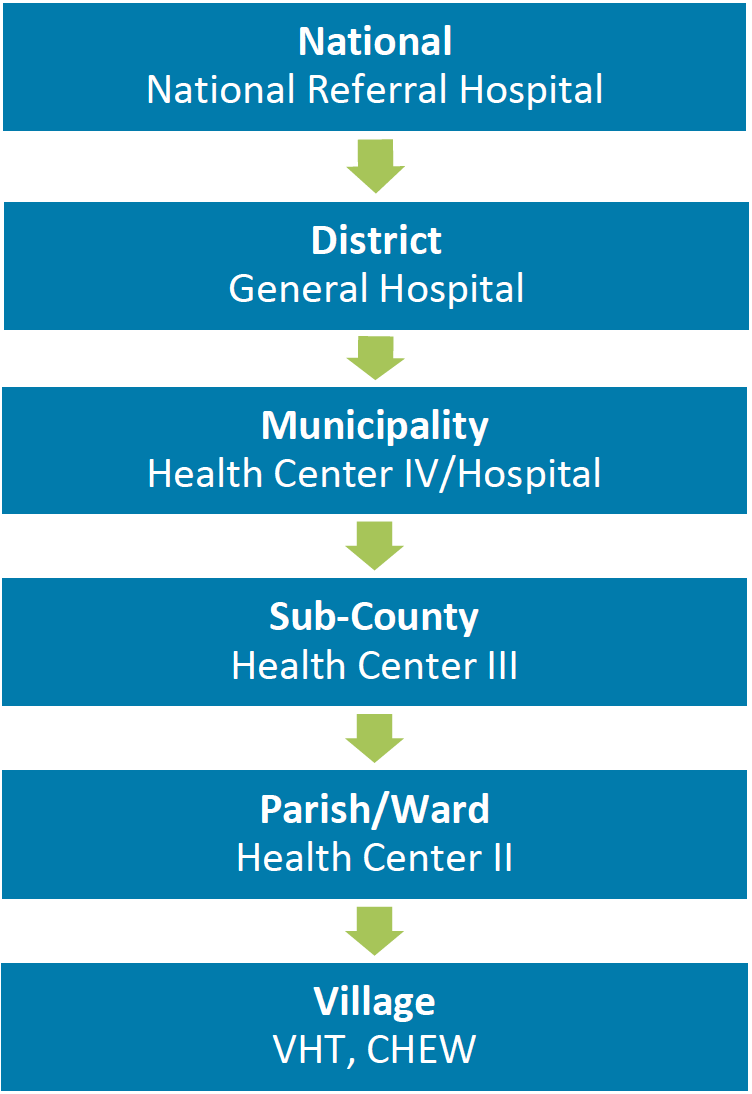
In Uganda, EPI is implemented through activities at static facilities and outreach sessions at locations within health facilities’ catchment areas. Supplementary immunization campaigns, including the Family Health Days program, held twice a year for a month at a time, focus on ZD and partially immunized children. During this time, communities are mobilized to reach children under 15 and their families for integrated health services, including health education, antenatal care, deworming, vitamin A supplementation, and routine immunization at health facilities and community-based sites.49 Static immunization services are delivered at sites across all levels and sectors of the health system. Given the decentralized structure of Uganda’s health system (Figure 13), districts and sub-districts are responsible for EPI service planning and delivery, while EPI policy and standards are established at the national level. VHTs and CHEWs mobilize communities for vaccination, plan outreach immunization sessions, and refer community members to static sites for immunization. Community members are typically referred to health centers at the parish-level and sub-county levels (health centers I and II) for immunization. However, patients may be referred to higher-level health facilities (e.g., III or IV) if lower-level facilities are unavailable.50
Figure 13. Organization of Uganda’s Health System
The Uganda National EPI was established in 1983 and its activities are funded by the public and private sectors, including the government, technical and financial partners, and NGOs. The EPI is a division of the Ministry of Health and falls under the Department of National Disease Control. In 2015, the Government of Uganda enacted the Public Private Partnership Act, which allows it to work with the private for- and nonprofit sectors to provide some social services, including immunization. The Uganda Health Federation establishes private sector accountability mechanisms and ensures adherence to national guidelines. Data from Uganda’s 2016–2020 cMYP indicate that 19 percent of all EPI service providers in the country are based at private and NGO clinics. As of 2018, approximately half of all health facilities in the country were private, and most were near Kampala in the Central region.51
Immunization Partners and Zero Dose Efforts
Table 4 below shows a list of immunization stakeholders engaged in ZD efforts in Uganda. This content will be expanded in future iterations of the landscape analysis through a series of KIIs with stakeholders at national and subnational levels.
Table 4. List of Preliminary Immunization Partners in Immunization
| Sl. No. | Organization/Entity | Category | Geographic coverage | Dates of work | Funder | Description of work |
|---|---|---|---|---|---|---|
| 1 | Makerere University School of Public Health | Research | National | 1922–present | Various, including USAID, BMGF, UNICEF, and WHO | To conduct research to increase access to reproductive and MNCH services, including vaccination. Uganda CLH member. |
| 2 | World Health Organization (WHO) | Funder/ technical assistance | International | 1950–present | WHO | To support health and development of Ugandans, including monitoring and assessing trends in health indicators. |
| 3 | United Nations International Children's Emergency Fund (UNICEF)- Uganda | Funder/ technical assistance | International | 1960–present | UNICEF | To support efforts to respond to the most vulnerable children, including by working with all levels of government to provide immunization services. |
| 4 | USAID | Funder | International | 1962– present | U.S. government | To strengthen capacity to deliver MNCH services, including immunization. |
| 5 | World Bank | Funder | International | 1963–present | International Development Association (IDA) | To support development including poverty reduction and economic recovery. |
| 6 | Uganda Virus Research Institute | Research and implementation | National | 1977–present | Government of Uganda | To conduct research on disease prevention and control, surveillance, and policy development. |
| 7 | Uganda Bureau of Statistics | Government | National | 1998–present | Government of Uganda | To promote reliable collection and analysis of data across all sectors. |
| 8 | Gavi | Funder | International | 2001–present | Gavi | To fund initiatives to vaccinate children against deadly and debilitating infectious diseases. |
| 9 | African Field Epidemiology Network (AFENET) | Technical assistance | International | 2005–present | MOH, BMGF, among others | To work with the MOH to strengthen the ability of Uganda’s public health system to monitor and respond to challenges. |
| 10 | Infectious Diseases Research Collaboration (IDRC) | Research | National | 2008–present | BMGF, Global Fund, Gavi, among others | To conduct research on infectious diseases, including measles and malaria. Uganda CLH member. |
| 11 | National Institute of Public Health | Government | National | 2013–present | Ministry of Health | To manage disease control activities. |
| 12 | Uganda National Immunization Technical Advisory Group (UNITAG) | Government | National | 2014–present | WHO | To guide immunization-related policy decisions. |
| 13 | PATH | Technical assistance | International | 2016–present | U.S. government, UNICEF, Gavi, WHO, among others | To support the development, delivery, and introduction of vaccines. Includes a focus on ZD children. Uganda CLH member. |
| 14 | MOMENTUM Integrated Health Resilience (MIHR) | Technical assistance | International | 2020–present | USAID | To increase availability and use of essential health services, including immunization, with a focus on eight districts of the country. |
Relevant Resources
Below are several relevant resources related to health and immunization in Uganda, including surveys, data, reports, and databases.
Surveys
Immunization and Health Data
Program Reports, National Strategies, and Databases
References
1 The DHS Program STATcompiler. Funded by USAID.
2 United Nations Inter-agency Group for Child Mortality Estimation (2023).
3 The DHS Program STATcompiler. Funded by USAID.
4 United Nations, Department of Economic and Social Affairs, Population Division. 2022. “World Population Prospects 2022, Online Edition.”
5 Li, X., Mukandavire, C., Cucunubá, Z. M., Londono, S. E., Abbas, K., Clapham, H. E., Jit, M., Johnson, H. L., Papadopoulos, T., Vynnycky, E., Brisson, M., Carter, E. D., Clark, A., Villiers, M. J. de, Eilertson, K., Ferrari, M. J., Gamkrelidze, I., Gaythorpe, K. A. M., Grassly, N. C., … Garske, T. (2021). Estimating the health impact of vaccination against ten pathogens in 98 low-income and middle-income countries from 2000 to 2030: A modelling study. The Lancet, 397(10272), 398–408.
6 Gavi Secretariat. 2022. “Uganda Zero Dose Analysis.” Unpublished.
7 Gavi Secretariat. 2023. “Uganda Zero Dose Analysis.” Unpublished.
8 Ibid.
9 Ibid.
10 Ibid.
11 https://covid19.gou.go.ug/cov/
12 Indirect effects of COVID-19 on maternal, neonatal, child, sexual and reproductive health services in Kampala, Uganda | BMJ Global Health. (n.d.). Retrieved July 20, 2023.
13 Ibid.
14 ICAP. (June 13, 2022). ICAP-Supported Study in Uganda Assesses What Drives or Delays Vaccination Uptake.
15 Asiimwe, D. (July 19, 2021). Keeping routine immunisation going during Uganda’s second lockdown. Vaccines Work. Gavi the Vaccine Alliance.
16 Agaba, J. (March 24, 2023). “We need to reach every child”: How Uganda’s routine immunisation program climbed back from COVID-19. Vaccines Work. Gavi the Vaccine Alliance.
17 Athiyaman, A., Ajayi, T., Mutuku, F., Luwaga, F., Bryer, S., Giwa, O., Mngemane, S., et al. (2023). Recovering from the Unprecedented Backsliding in Immunization Coverage: Learnings from Country Programming in Five Countries through the Past Two Years of COVID-19 Pandemic Disruptions. Vaccines, 11(2), 375. MDPI AG.
18 Uganda Bureau of Statistics - UBOS and ICF. 2018. Uganda Demographic and Health Survey 2016. Kampala, Uganda and Rockville, Maryland, USA: UBOS and ICF.
19 Rahimi, A., Kassam, R., Dang, Z., & Sekiwunga, R. (2019). Challenges with accessing health care for young children presumed to have malaria in the rural district of Butaleja, Uganda: A qualitative study. Pharmacy Practice, 17(4), 1622.
20 Dowhaniuk, N. (2021). Exploring country-wide equitable government health care facility access in Uganda. International Journal for Equity in Health, 20(1), 38.
21 Uganda Bureau of Statistics (UBOS). Uganda Population and Housing Census 2014—Provisional Results. Revised edition. UBOS; 2014.
22 Uganda Comprehensive Refugee Response Portal. UNHCR.
23 Kamya, C., F. Namugaya, C. Opio, P. Katamba, E. Carnahan, A. Katahoire, J. Nankabirwa, J. Okiring, P. Waiswa. Global Health: Science and Practice Aug 2022, 10 (4) e2100663; DOI: 10.9745/GHSP-D-21-00663.
24 Evaluation Team. Evaluation of the Drivers of Urban Immunization in Uganda: A case study of Kampala city, Kampala, Uganda: IDRC; 2020. Infectious Diseases Research Collaboration 2C Nakasero Hill Road.
25 Dowhaniuk, N. (2021). Exploring country-wide equitable government health care facility access in Uganda. International Journal for Equity in Health, 20(1), 38.
26 Devlin, Kristen, Kimberly Farnham Egan, and Tanvi Pandit-Rajani, “Community Health Systems Catalog Country Profile: Uganda.,” Advancing Partners & Communities., Arlington, VA, 2016.
27 WHO Global Health Expenditure Database. Health Expenditure Profile, Uganda.
28 Arsenault, Catherine, Mira Johri, Arijit Nandi, José M. Mendoza Rodríguez, Peter M. Hansen, and Sam Harper. 2017. “Country-Level Predictors of Vaccination Coverage and Inequalities in Gavi-Supported Countries.” Vaccine 35 (18): 2479–88.
29 Wagstaff, Adam, Patrick Eozenou, and Marc Smitz. 2019. “Out-of-Pocket Expenditures on Health,” April.
30 World Health Organization. 2021. “Global Expenditure on Health: Public Spending on the Rise?” Global Report.
31 Sim, So Yoon, Elizabeth Watts, Dagna Constenla, Logan Brenzel, and Bryan N. Patenaude. 2020. “Return On Investment From Immunization Against 10 Pathogens In 94 Low- And Middle-Income Countries, 2011–30.” Health Affairs 39 (8): 1343–53.
32 WHO Immunization Data Portal.
34 The Uganda National Expanded Programme on Immunisation Multi-Year Plan 2016–2020. Uganda Ministry of Health.
35 Devlin, Kristen, Kimberly Farnham Egan, and Tanvi Pandit-Rajani, “Community Health Systems Catalog Country Profile: Uganda.” Advancing Partners & Communities., Arlington, VA, 2016.
36 National Human Resources for Health Dashboard.
37 The National Health Workforce Accounts database, World Health Organization, Geneva.
38 Community Health Extension Workers National Strategy 2018–2022. Ministry of Health.
39 Ibid.
40 Kintu P, Nanyunja M, Nzabanita A, Magoola R: Development of HMIS in poor countries: Uganda as a case study. Health Policy Dev. 2005, 3 (1): 46-53.
41 Wandera, S. O., Kwagala, B., Nankinga, O., Ndugga, P., & Kabagenyi, A. (2018). Integrating Family Planning Data in Uganda’s Health Management Information System.
42 Kiberu, V.M., Matovu, J.K., Makumbi, F. et al. Strengthening district-based health reporting through the district health management information software system: the Ugandan experience. BMC Med Inform Decis Mak 14, 40 (2014).
43 National and subnational coverage and other service statistics for reproductive, maternal, newborn and child health from health facility data and surveys. Countdown to 2030/GFF/UNICEF/WHO workshop. June 2022.
44 MOH. National Technical Guidelines for Integrated Disease Surveillance and Response - Third Edition. 2021.
45 Nansikombi, H. T., Kwesiga, B., Aceng, F. L., Ario, A. R., Bulage, L., & Arinaitwe, E. S. (2023). Timeliness and completeness of weekly surveillance data reporting on epidemic prone diseases in Uganda, 2020–2021. BMC Public Health, 23, 647.
46 Ward, K., Mugenyi, K., Benke, A., Luzze, H., Kyozira, C., Immaculate, A., Tanifum, P., Kisakye, A., Bloland, P., & MacNeil, A. (2017). Enhancing Workforce Capacity to Improve Vaccination Data Quality, Uganda. Emerging Infectious Diseases, 23(Suppl 1), S85–S93.
47 Greene, J., & Samplin-Salgado, M. (n.d.). AUTHOR: Michelle Choy SUPPORT: Richard Kintu (Last Mile Health), Kyle Muther (Last Mile Health), Kenneth Mugumya (Last Mile Health), and Peter Kaddu (Last Mile Health).
48 Devlin, Kristen, Kimberly Farnham Egan, and Tanvi Pandit-Rajani, “Community Health Systems Catalog Country Profile: Uganda.,” Advancing Partners & Communities., Arlington, VA, 2016.
49 Health workers use special days to reach every child with life-saving vaccines | UNICEF Uganda. (n.d.). Retrieved August 23, 2023.
50 Mariam Basajja, Mutwalibi Nambobi; Information Streams in Health Facilities: The Case of Uganda. Data Intelligence 2022; 4 (4): 882–898.
51 National Health Facility Master List 2018. Division of Health Information, Uganda.