Bangladesh Zero-Dose Landscape

Background
The Gavi Zero-Dose Learning Hub (ZDLH) is responsible for highlighting work and outputs generated by the four Gavi Country Learning Hubs (CLHs) in Bangladesh, Mali, Nigeria, and Uganda with the objective of using this evidence to better understand the factors influencing implementation and performance of approaches to identify and reach zero-dose (ZD) and under-immunized children as well as missed communities. The consortium is led by JSI Research & Training Institute, Inc. (JSI) in partnership with the Indian Institute of Health Management Research (IIHMR) and The Geneva Learning Foundation (TGLF). Together, the group aims to support CLHs to implement Gavi's Identification-Reach-Monitoring-Measurement-Advocacy (IRMMA) framework; facilitate sharing and learning across the CLHs; contribute evidence to capture, synthesize, and disseminate the breadth of learning across the Gavi Alliance; and ultimately help improve immunization equity and reduce the number of ZD and under-immunized children globally by facilitating quality evidence generation and uptake.
In pursuit of these objectives, the ZDLH has developed ZD landscapes to synthesize the evidence to date on immunization prevalence, policy, and programming in each of the four learning hub countries. These landscapes describe the current immunization and ZD context, including coverage trends, equity, health systems, and existing partners and programming to orient implementers and funders to the broad immunization context and opportunity for intervention to reduce the prevalence of ZD children. While these landscapes present the findings of syntheses of existing literature, the CLHs in Bangladesh and other countries will generate evidence based on their own country-level ZD programming and activities such as rapid assessments and surveys.
The purpose of this landscape is to provide the Bangladesh CLH and stakeholders in Bangladesh with a comprehensive overview of the immunization landscape within the country, with a special focus on ZD and under-immunized children. Given the highly variable and contextual nature of the drivers, barriers, and programmatic approaches to reach ZD and under-immunized children, it is important to understand the unique context, policies, and economics of the country to help guide approaches, but also to better understand and interpret why changes in IRMMA may or may not occur. This landscape also aims to inform research and programming efforts in Bangladesh by identifying important knowledge gaps that pertain to the IRMMA framework for ZD and under-immunized children.
Methods
The ZD landscape assessments are based on literature reviews and secondary data analyses. To identify relevant literature, the ZDLH team searched both gray and peer-reviewed sources, ministry and partner websites, and existing Gavi reviews and resources. Domains of interest included immunization coverage and equity as well as information about the health system in which the immunization program operates including, but not limited to, human resources, financing, immunization policies, and the health system structure. Relevant publications were identified and reviewed and information related to the ZD or immunization context in each country was extracted. Where gaps in information remain, the team relies on input from CLHs and key informant interviews (KIIs) conducted as part of the complementary political economy analysis. These landscapes are intended to represent the current situation in the countries and, therefore, will be updated on an annual basis to include new resources including those generated by the CLHs.
Introduction
Bangladesh has made tremendous progress over the last 20 years ensuring that children in the country are immunized against diseases that previously made up a large proportion of childhood illness and death, including diphtheria, tetanus, and measles. For the past 10 years, Bangladesh has been among the 64 percent of countries that have achieved the target of 90 percent immunization coverage or higher.1 Presently, the focus in Bangladesh is to address the “last mile:” reaching all eligible children with routine vaccines as per the national immunization schedule. This includes reaching ZD and under-immunized children in rural and hard-to-reach areas including hilly areas and communities accessible only by boat, urban slums, and locations with refugee and migrant populations, also known as missed communities. These children, who are also at higher risk for other illnesses and malnutrition, can be difficult to locate, but identifying and reaching them is an essential step toward full and equitable immunization coverage in the country.2
Bangladesh, which shares borders with India and Myanmar (Figure 1), is one of the most densely populated countries in the world with an estimated population of 169 million people in 2021, of which approximately 14.6 million are children under five (Table 1).3
Figure 1. Map of Bangladesh

Table 1. Total Population and Residence
| Total Population (2021) | |
|---|---|
| Total | 169,356,251 |
| Male | 83,998,088 (49.6%) |
| Female | 85,358,163 (50.4%) |
| Residence (2021) | |
|---|---|
| Rural | 61% |
| Urban | 39% |
Source: United Nations, Department of Economic and Social Affairs, Population Division. 2022. “World Population Prospects 2022, Online Edition.”
Despite recent progress toward reducing mortality in children under five in Bangladesh (Figure 2), the United Nations Inter-agency Group for Child Mortality Estimation (UN-IGME) estimates that 82,000 children died in 2021, many from preventable causes, including vaccine-preventable diseases.4
Source: “Levels & Trends in Child Mortality: Report 2022.” 2023. Estimates Developed by the United Nations Inter-Agency Group for Child Mortality Estimation. United Nations Children’s Fund, World Health Organization, World Bank Group, United Nations.
The 2018 Bangladesh Report on Vital Statistics indicated that pneumonia and respiratory diseases, some of which may be prevented by vaccines, accounted for nearly half of all deaths of children under five in the country (Figure 3).*5
Source: Bangladesh Bureau of Statistics. 2019. “Report on Bangladesh Sample Vital Statistics 2018.” Bangladesh: Ministry of Planning, Statistics and Informatics Division.
Improved access to immunization is a principal driver of the decrease in under-five mortality in developing countries. Three decades of routine immunization programs have produced dramatic declines in vaccine-preventable diseases such as measles in countries like Bangladesh (Figure 4).
Source: ICF, 2015. The DHS Program STATcompiler. Funded by USAID. March 15 2023; Institute for Health Metrics and Evaluation (IHME). Global Burden of Disease Study (GBD 2019). Seattle, WA: IHME; 2023. Accessed March, 2023. Figure updated and adapted from What did Bangladesh do? (n.d.). Exemplars in Global Health: Bangladesh. Retrieved March 10, 2023.
* The data from the Sample Vital Statistics report represent the most recent publicly available data regarding the cause of death among children under five in Bangladesh. However, given the large proportion that fall into the “other” category and lack of raw data for re-analysis, we urge caution when interpreting these results.
Immunization Context
Despite high overall coverage of childhood vaccination in Bangladesh, immunization gaps remain with some children missing doses or not receiving any vaccinations. Households that include children who have not received a single dose of the pentavalent vaccine series are estimated by a recent Gavi analysis of immunization coverage data to represent six percent of all deaths (6,046 total deaths) among children under five in the country.†6 Operationally, Gavi defines a ZD child as one who has not received a single dose of a diphtheria, tetanus, and pertussis-containing vaccine.
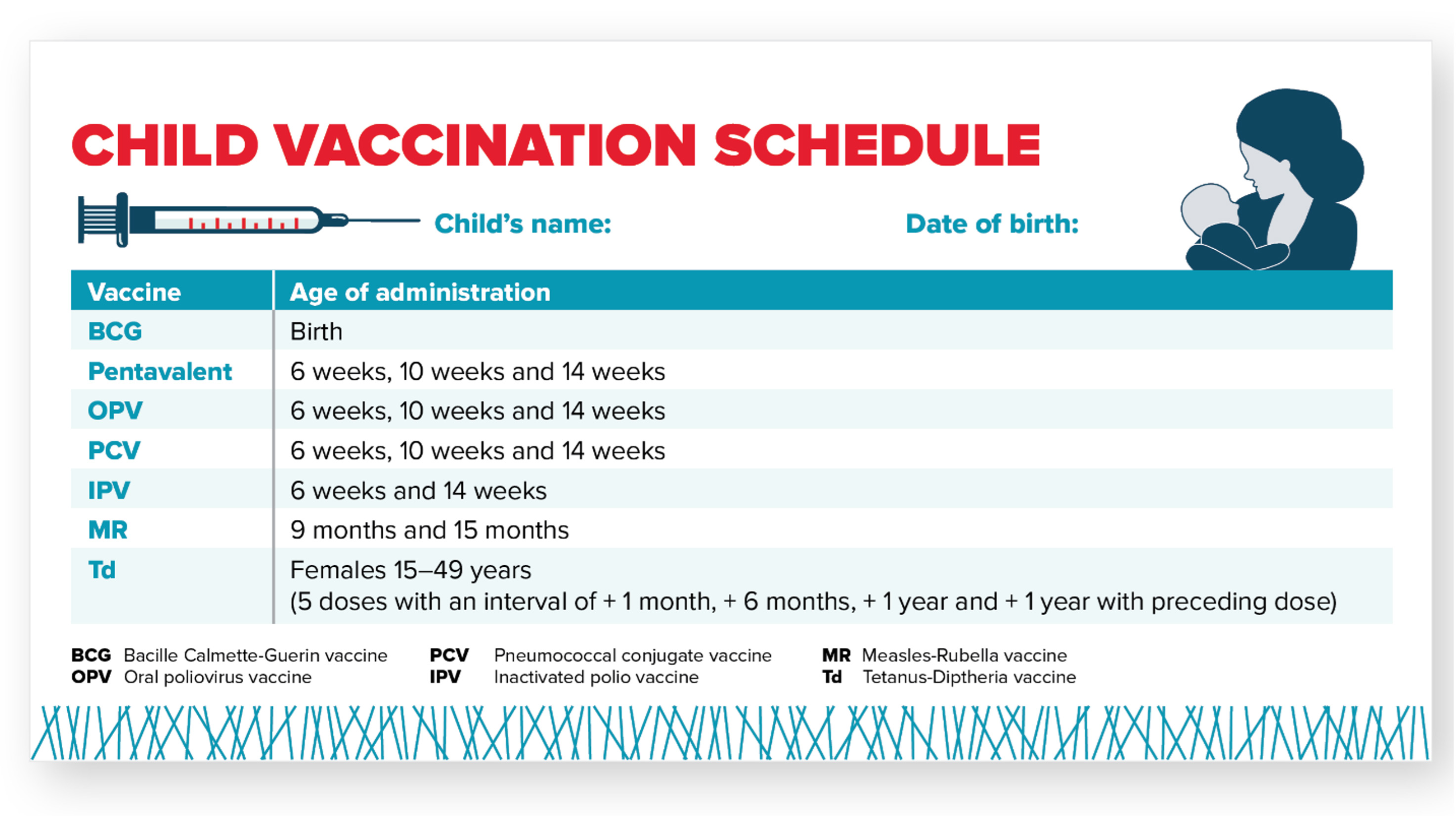
Immunization Schedule
Bangladesh’s current immunization schedule includes 10 different vaccines and targets 3.8 million children each year (Figure 5). Bangladesh administers the pentavalent (penta) vaccine, which protects against diphtheria, tetanus, pertussis, hepatitis B, and Haemophilus influenzae type b (Hib). In Bangladesh and for the purposes of this landscape, ZD children are defined as children who have not received a single dose of the pentavalent vaccine series.
Figure 5. Bangladesh Childhood Vaccination Schedule
Coverage Estimates
Current coverage estimates for six basic immunizations in Bangladesh are presented in Figure 6. Coverage ranges from 99 percent of children receiving Bacillus Calmette–Guérin (BCG) at birth to 93 percent of children receiving the second dose of a measles containing vaccine (MCV) at 15 months of age. Despite the current high coverage across antigens, Bangladesh could prevent an estimated 342,600 future deaths through further scale up of preventive immunization activities between 2022-2025.7
Source: World Health Organization/UNICEF Estimates of National Immunization Coverage (WUENIC)—2021 estimates. (2022). WHO Immunization Data Portal.
Estimating the number of ZD children in Bangladesh requires estimates of Penta1 coverage and the total number of surviving infants. These numbers can vary based on the source of the data, resulting in different estimates of the ZD population (Table 2). Positive estimates (those above zero) range from 14,789 (from the Institute for Health Metrics and Evaluation [IHME]) to 29,577 ZD children (WHO/UNICEF Estimates of National Immunization Coverage [WUENIC]).8
Table 2. Bangladesh ZD Estimate Inputs
| Source | Total Number of Surviving Infants | Penta 1 Coverage | Number of ZD Children |
|---|---|---|---|
| WUENIC (2021) | 2,957,723 | 99% | 29,577 |
| IHME (2021) | 2,957,723 | 100% | 14,789 |
Source: Gavi Secretariat. 2023. “Bangladesh Zero Dose Analysis.” Unpublished.
Administrative data from national sources estimate Penta1 coverage at above 100 percent, resulting in a negative number of ZD children. The quality of administrative data can be problematic, evidenced by coverage rates of over 100 percent, which indicates either an error in the documentation of the number of children receiving Penta1 vaccines (numerator) or in the estimates of the total number of children (denominator). The National Immunization Strategy (2023-2027) suggests that the denominators used are likely an underestimate based on data from a 2011 census and that these estimates will be updated when the next census takes place.9 For this reason, Table 2 does not include ZD estimates derived from administrative data.
The goal of WUENIC analyses is to provide national immunization estimates on an annual basis. WUENIC immunization estimates are developed by triangulating data from several sources including government data, published and unpublished survey data, and consultation with local experts and governments. Statistical and mathematical modeling are not used to derive the final coverage estimates and estimates are not available at the sub-national level.10 As such, WUENIC estimates are not useful for identifying the location of ZD children in the country, but are useful for looking at trends in the ZD population over time.
IHME projections include different inputs and analyses because the goal of these estimates is different from those of WUENIC or administrative data. The goal of IHME is to generate highly-specific geospatial estimates of immunization coverage that are combined with additional data to generate national coverage estimates. IHME, like WUENIC, uses household survey data as well as national data, but it also uses covariates of immunization (such as residence or mother’s level of education) when calculating estimates. Using this data, IHME models immunization coverage at a hyper-local level (a five-by-five kilometer [km] area) and then incorporates additional higher-level data to model a national estimate.11 The resulting estimates provide more insight into the probable locations of ZD children within a country, but also include more assumptions and potential error than estimates generated from household surveys or administrative data.
Given the differences in source data and estimation approaches, the true number (and location) of ZD children is not known. However, by triangulating the various estimates, we can determine where there is overlap and generate an informed best guess that can be used for broad planning purposes. Tailored implementation strategies to vaccinate ZD children may require other methods to better understand where they are located, how to reach them, and how to effectively bring them into routine immunization services.
For the purposes of this landscape, we will use data from both WUENIC and IHME sources with the understanding that the estimates are imperfect. Data from household surveys, like the Bangladesh Demographic and Health Surveys (DHS), will also be incorporated into this assessment, particularly for equity analyses.
Effects of the COVID-19 Pandemic
In March 2020, Bangladesh joined the global effort to curb the spread of COVID-19 by instituting a series of lockdowns, including a two-month national lockdown from March until May of 2020. During this time, routine immunization services, including outreach sessions, were significantly scaled back and, in some cases, all but eliminated.12 Studies from Bangladesh, and globally, suggest that in most locations, immunization services were re-instated to near normal levels in the months that followed and catch-up campaigns were conducted in earnest. However, a study by Hanifi et al. estimates that 3.2 million children in Bangladesh may have missed scheduled vaccines during that period.13, 14 While services were re-instated after the initial lock-down, a health worker strike in November and December of 2020 also likely contributed to decreases in pentavalent, measles, and BCG coverage because Expanded Programme on Immunization (EPI) sites scaled back services during this period (Figure 7).15
Figure 7. COVID-19 Effects: Number of EPI Sites Reporting Vaccinations over Time by Type
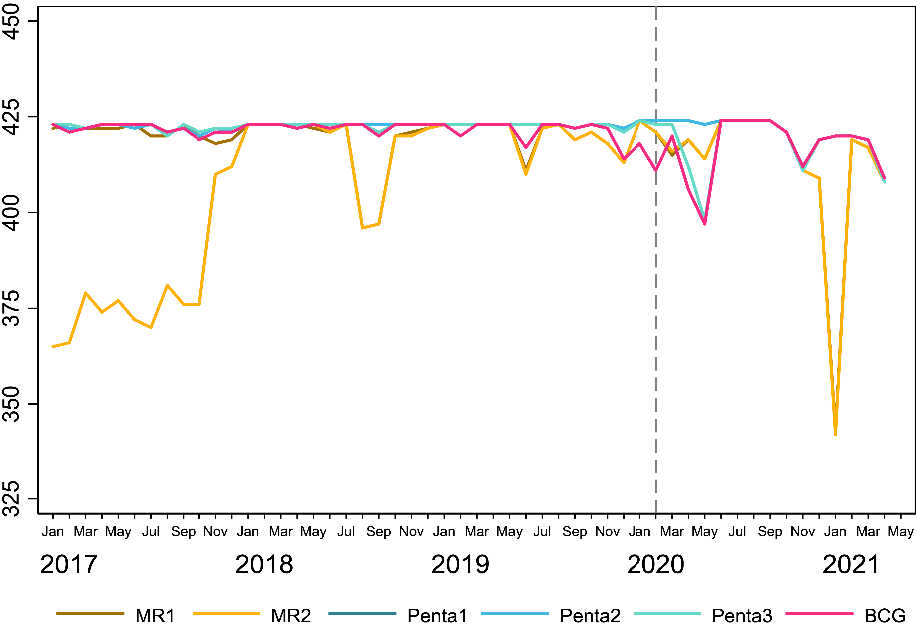
Source: Angeles, Gustavo, Hannah Silverstein, Kara Zunaid Ahsan, Mohammad Kibria, Nibras Ar Rakib, and Gabriela Escudero. 2021. “Estimating the Effects of COVID-19 on Immunization Services Use in Bangladesh.” Data for Impact, United States Agency for International Development.
Finally, the pandemic affected other aspects of the immunization system in Bangladesh. For example, planned activities, like the 2021 census, that would help inform immunization planning and generate more accurate denominators for monitoring purposes, have been postponed.16
† Note: These deaths are not all attributable to vaccine preventable diseases, but represent all-cause mortality among this population which is particularly vulnerable to morbidity and mortality from other causes, like malnutrition.
Equity
Gavi’s 5.0 strategy to identify and reach ZD and under-immunized children focuses on equity. To comprehensively implement Gavi’s 5.0 strategy, it is essential to examine the contexts in which ZD and under-immunized children live.
Factors Influencing ZD Status
Figure 8 presents sociodemographic characteristics for children who did not receive Penta1, BCG, and measles vaccines. These three antigens, given at different times and different locations, can represent different immunization access barriers. The pentavalent vaccine series is typically used as a proxy indicator of access to routine immunization because it is given during well-child visits at 6, 10, and 14 weeks.
The measles vaccine, however, is given first at 9 months and then again at 15 months in Bangladesh, usually at well-child check-ups at the community level, which also represents access to routine immunization services, albeit at a later age. BCG is given at birth in Bangladesh, so its coverage may better represent birth in a health facility than access to routine immunization services.
Sources: 1) WHO. Measles vaccination status and sociodemographic characteristics. Trend and factors affecting zero-vaccination status of children for measles-containing vaccine in Bangladesh: Analysis from two recent demographic and health surveys. World Health Organization, Regional Office for South-East Asia. New Delhi. Retrieved 16.02.2023.
2). National Institute of Population Research and Training (NIPORT), and ICF. 2020. Bangladesh Demographic and Health Survey 2017-18. Dhaka, Bangladesh, and Rockville, Maryland, USA: NIPORT and ICF.
The data presented in Figure 8 and additional existing literature indicate that the mother’s education, the number of antenatal care (ANC) visits she attended during her last pregnancy, household wealth, and where a child lives are the most important predictors of whether a child will receive Penta1 in Bangladesh.17, 18 Children whose mothers had no education or only primary level education are more likely to be ZD children than those whose mothers completed secondary or higher education. Children from the poorest households are more likely to be unvaccinated than children in wealthier households.19 Additionally, the mother’s interaction with the health system during pregnancy is also correlated with children’s immunization. Children of mothers who did not receive the recommended four or more antenatal care visits during their last pregnancy were more likely to be unvaccinated than children of mothers who attended the recommended number of visits.20, 21 Finally, geographic location is an important predictor of immunization status. Among all the administrative divisions, a greater proportion of children in Sylhet were ZD (4.2 percent) compared with children in Rajshahi (0 percent) and Khulna (0 percent). As the map below indicates, more ZD cases are located in the eastern part of the country.22 Data from IHME (2020) also suggest that the highest number of ZD children can be found in Sylhet and Chittagong and around the urban areas of Dhaka (Figure 9). Studies in the peer-reviewed literature from Bangladesh also report that geography is a determinant of immunization coverage. One study by Uddin et al. in urban slums surrounding Dhaka city indicated that full immunization coverage was dramatically lower in the slums when compared with coverage at the national level.23
Figure 9. Number of ZD Children by District
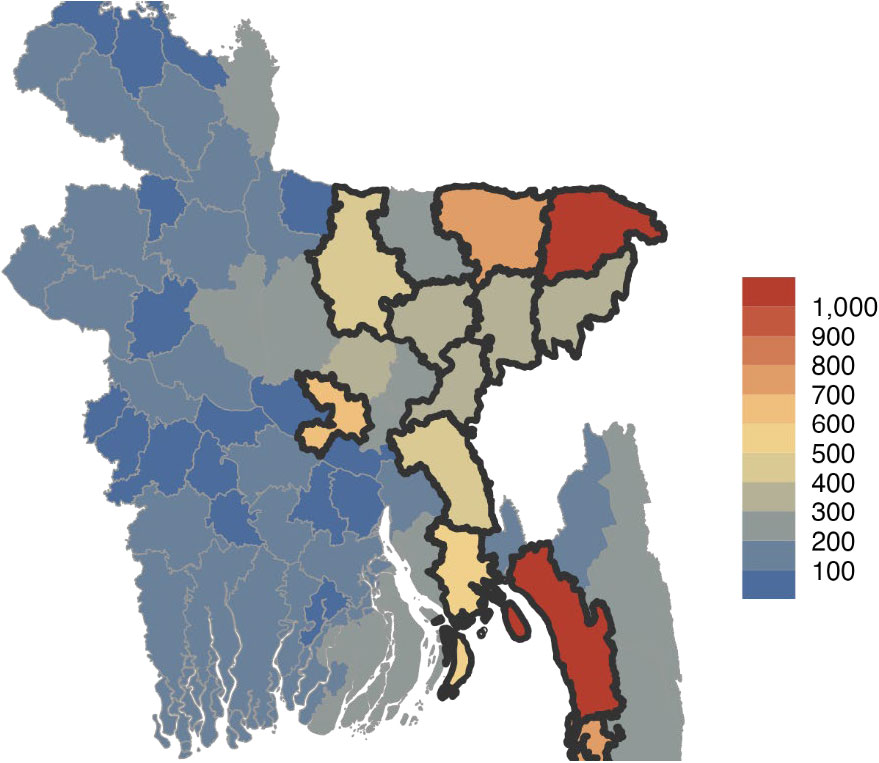
Source: IHME 2021 data cited in Gavi Secretariat. 2023. “Bangladesh Zero Dose Analysis.” Unpublished.
Studies among marginalized populations within Bangladesh have also tried to identify ZD and under-immunized children living in the country. One study examined seroprevalence among forcibly displaced Rohingya children living in both formal refugee camps as well as makeshift camps. Make-shift camps are more informal settlements that are less likely to provide healthcare, including routine immunization services. The analysis indicated that of children ages one to six years living in makeshift camps, 92 percent (CI: 84-96) had received at least one dose of a DPT-containing vaccine (i.e., either DPT or the pentavalent vaccine) compared with 98 percent (CI: 95-99) of children ages one to six years living in the more formal settlement.24 This finding was supported in a similar study comparing Rohingya refugees living in formal and informal settlements.25 Younger children (one to six years of age) were less likely than older children (7-14 years of age) to show sero-protection (the result of immunization or illness with the disease) and the authors hypothesized that this was because older children received vaccinations in Myanmar before health services in Rakhine state began to decline due to violence against Rohingya populations. Additionally, when asked why children did not participate in immunization campaigns, caregivers noted that they were not aware of campaigns or that children were unavailable (away due to school, daycare, or labor). A study by Jalloh et al. (2018) also examined factors contributing to lack of uptake of immunization services among Rohingya refugees in Bangladesh. While caregivers understood the importance of immunization for their children, beliefs about the side effects were a barrier to immunization uptake.26
While a number of publications include qualitative inquiry into vaccine hesitancy in Bangladesh, most focus on special populations (like refugees and migrants). Current, qualitative research among families of ZD and under-immunized children and missed communities including ethnic minorities, geographically remote communities, urban slum populations, and other vulnerable groups constitutes a gap in the research.
Health Systems
Bangladesh has a pluralistic health system, comprised of government, private sector, and donor agencies and non-governmental organizations (NGOs). Figure 10 shows that overall, expenditure on healthcare, including government spending, has increased in Bangladesh over the last 20 years from $12 per capita in 2004 to $51 per capita in 2020, although the percentage of GDP has remained steady between two and three percent.27
Source: World Health Organization. 2022. “Global Health Expenditure Database- 2022 Release.” January 24, 2022.
When compared with other countries in the region, Bangladesh only spends slightly more per capita on healthcare than Pakistan (Figure 11).
Source: “Bangladesh Healthcare Spending 2000-2023.” 2023. Accessed March 3, 2023.
However, a better predictor of high immunization coverage is the combination of higher levels of government spending as a proportion of total spending on healthcare and low out-of-pocket spending.28 This is because greater government investment in programs, like routine immunization, and lower out-of-pocket costs for immunization make it more accessible to children from the poorest households and their families.29 In both metrics, Bangladesh has regressed in the past 20 years. Government spending as a proportion of total spending has dropped from 21.9 percent to 18 percent between 2005 and 2020 and out-of-pocket spending as a proportion of total spending has risen from 65 percent to 74 percent during the same time period (Figure 12). This stagnation in government spending and increase in out-of-pocket spending over the past 20 years aligns with trends seen in other lower-middle income countries globally.30
Source: World Health Organization. 2022. “Global Health Expenditure Database- 2022 Release.” January 24, 2022.
Immunization Financing
Immunization is one of the most important and cost-effective public health interventions. According to one study, for every United States (U.S.) dollar spent on immunization between 2011 and 2020, there was an average return of up to U.S. $26 dollars across a child’s lifetime.31 In 2021, Bangladesh spent U.S. $72 million dollars on vaccines and routine immunization services, of which 46 percent was financed by the government and 54 percent was financed by external funders.32
Donor Support
Currently, Gavi is the largest source of external financing for immunization in Bangladesh, but this support is scheduled to phase out by 2026, as the country has exceeded the set threshold for Gavi support and will transition to self-financing for immunization. In 2018, Gavi provided nearly U.S. $60 million dollars in immunization programming support, largely in the form of health system strengthening funds and new and under-used vaccine support for pneumococcal conjugate vaccine, pentavalent, inactivated poliovirus (IPV), and measles vaccines (Figure 13).
Source: Gavi, the Vaccine Alliance Disbursement Data, 2022.
In addition to Gavi, important development partners for immunization in Bangladesh include United Nations Children’s Fund (UNICEF), World Health Organization (WHO), World Bank, United States Agency for International Development (USAID), and UK Aid Direct.33 In Bangladesh, most of the responsibility for routine immunization services (including managing the routine public immunization schedule and conducting immunization campaigns) falls under the National Immunization Program, which is situated under the Directorate-General of Health Services within the Ministry of Health and Family Welfare (MoHFW). Bangladesh also has a National Immunization Technical Advisory Group, called the National Committee for Immunization Practice, which is made up of experts in pediatrics, infectious disease, epidemiology, and other relevant fields to provide technical recommendations to the ministry regarding routine immunization schedules and new vaccine introduction.
Other government agencies, such as the Directorate General of Drug Administration, are responsible for activities related to regulation and licensing of vaccines within the country. The Interagency Coordinating Committee (ICC) is responsible for coordinating resources and acting as a liaison between national agencies and international organizations, including Gavi. The ICC is made up of NGO stakeholders working in the country and representatives from different government agencies and is chaired by the Secretary of the MoHFW.
National Policies
Bangladesh’s latest National Immunization Strategy (NIS) is the main document the government produces that provides insight into immunization-related priorities. The latest NIS outlines immunization programming and priorities for the Bangladesh EPI for the period of 2023-2027. The strategy describes recent immunization achievements including maintenance of polio and maternal and neonatal tetanus (MNT) elimination statuses and maintenance of high immunization coverage levels and reduction in drop-out rates. It also highlights remaining gaps such as human resource shortages, including supply chain management staff, dependence on donor funding for training and the surveillance network, and the continued existence of areas deemed “hard-to-reach” for immunization efforts. National objectives set forth in the plan include maintaining high coverage rates, keeping the country free of polio and MNT, elimination of measles and rubella, maintaining hepatitis B control, and maintaining crucial aspects of immunization operations through the transition from external to government and domestic funding sources. The strategies for the immunization program outlined in the NIS to achieve immunization objectives contains one strategy of particular relevance to ZD programming efforts. The strategy includes identifying and implementing “creative approaches” in order to reach under-immunized, ZD, and missed communities in traditionally hard to reach areas, including urban slums, and other marginalized populations, including refugees and ethnic minorities. The focus on ZD children in the five-year strategy signals a commitment by the government to improve coverage and access among these populations.34
More generally, the inclusion of immunization activities in national strategy and policy documents indicates a commitment by the government to reduce vaccine preventable disease nationally. Table 3 summarizes key government documents that address the importance of immunization and outline specific activities and targets.
Table 3. National Policy and Strategy Documents Relevant to Immunization
| Policy/Legislation | Year/s | Summary |
|---|---|---|
| Bangladesh 8th Five-Year Plan | 2020-2025 | The government’s comprehensive five-year economic plan that details investments across sectors, including health. The plan sets forth future immunization targets, including 98 percent of children vaccinated with all basic vaccines by 2025 and 100 percent of children vaccinated by 2030. The plan also outlines priority interventions for child health, including focusing on routine immunization and disease surveillance in tandem with supplementary immunization activities like national immunization days and measles/tetanus campaigns. |
| The Health, Nutrition and Population Strategic Investment Plan (HNPSIP) | 2016-2021 | A comprehensive plan developed by the Government of Bangladesh to improve the health, population, and nutrition status of the country's population. The plan covers a five-year period and is updated periodically to reflect changing health needs and priorities. The main objectives of the HNPSIP include reducing maternal and child mortality, improving the health of the population, and addressing key health and nutrition challenges such as malnutrition and communicable diseases. As such, several activities detailed in the plan refer to immunization-related programming and policies. |
| National Urban Health Strategy | 2014 | Developed by the Ministry of Local Government, Rural Development and Cooperatives, this strategy highlights that the same upward trends in immunization coverage reported in some areas are not seen in urban slums and lists strengthening the preventive and primary health care management system as a key activity of the strategy, although immunization is not listed specifically. |
| Ending Preventable Child Deaths by 2035: Bangladesh Call for Action | 2013 | The declaration, made in 2013, as the follow up to the UNICEF Child Survival Call for Action, commits to reducing the under-five mortality rate to 20 deaths per 1,000 live births by 2035. Introduction of new vaccines is one of the seven strategic interventions listed to achieve this target. |
| National Health Policy | 2008 | The policy was developed by the MoHFW and was last updated in 2011. The key objectives of the National Health Policy of Bangladesh include improving access to quality health services, reducing health inequalities, and promoting public-private partnerships to improve the overall health system in the country. The plan also establishes health as a right of citizens of Bangladesh and advocates for equitable access to health care regardless of gender, disability, or socioeconomic level. |
| The National Immunization Policy of Bangladesh | 1979 | The plan aims to provide a comprehensive immunization program to reduce vaccine-preventable diseases and the morbidity and mortality associated with these diseases. The policy provides guidelines for the immunization of infants, children, adolescents, and adults, and emphasizes the importance of providing universal access to vaccines. The policy also prioritizes the use of vaccines with proven efficacy and safety, and ensures that all vaccines used in the country meet international quality standards. |
Human Resources for Health
Adequate human resources are essential for all health care services, including immunization services. However, immunization programs required a range of staff, including clinicians, supply chain professionals, logisticians, cold chain technicians, and data entry staff. While data are lacking on adequate staffing of non-clinical professionals who support immunization programs, data on clinical professionals shows growth in recent years. The comprehensive multi-year plan 2018-2022 for the National Immunization Program of Bangladesh details “considerable recruitment” of doctors, nurses, midwives, and community health workers, reducing vacancy rates from 20 percent in 2011 to 15 percent in 2018.35 Data from the WHO National Health Workforce Accounts database indicate that between 2003 and 2021 the ratio of nursing and midwifery personnel to patients increased from 2.7 per 10,000 people to 6.1 per 10,000 people. Additionally, the number of community health workers rose from 21,000 in 2005 to more than 148,000 in 2020.36 Despite these gains, adequate staffing is lacking in rural and hard-to-reach areas.37 Additionally, a 2014 analysis on health system bottlenecks to immunization found that the health workforce was classified as a “significant” or “major” bottleneck in the areas of vaccine introduction, service delivery, surveillance and cold chain, and effective vaccine management.38 This finding is supported in the 2023-2027 NIS which notes that currently 20 percent of all posts in the health system are currently vacant.39
Evidence related to current human resources and staffing for immunization services, particularly in rural and hard-to-reach areas, is missing from the published literature. This may be an area for further inquiry by the CLHs.
Health Management Information System Structure and Disaggregation, Data Availability and Use:
Bangladesh has utilized District Health Information Software 2 (DHIS2) as its health management information system (HMIS) for nearly 15 years and is one of the largest deployers of the system in the world, with average reporting rates exceeding 98 percent.40 In 2009, when the DHIS2 system was first established in Bangladesh, immunization data was one of the first sets of separate, program-based management information systems within the country to be incorporated into the larger system. Immunization is now one of many programs feeding data into the system from the community level up, with a reporting rate of 100 percent (Figure 14). In addition to public facilities, the country initiated a plan in 2013 to extend use of the HMIS to private facilities, NGOs, and city corporations starting with immunization data. Bangladesh also holds the distinction as the first country in the world to integrate cold chain data into the DHIS2 and is the only country (as of 2019) to have integrated all routine immunization and immunization supply chain data into DHIS2.
Figure 14. Bangladesh DHIS2 Reporting Structure
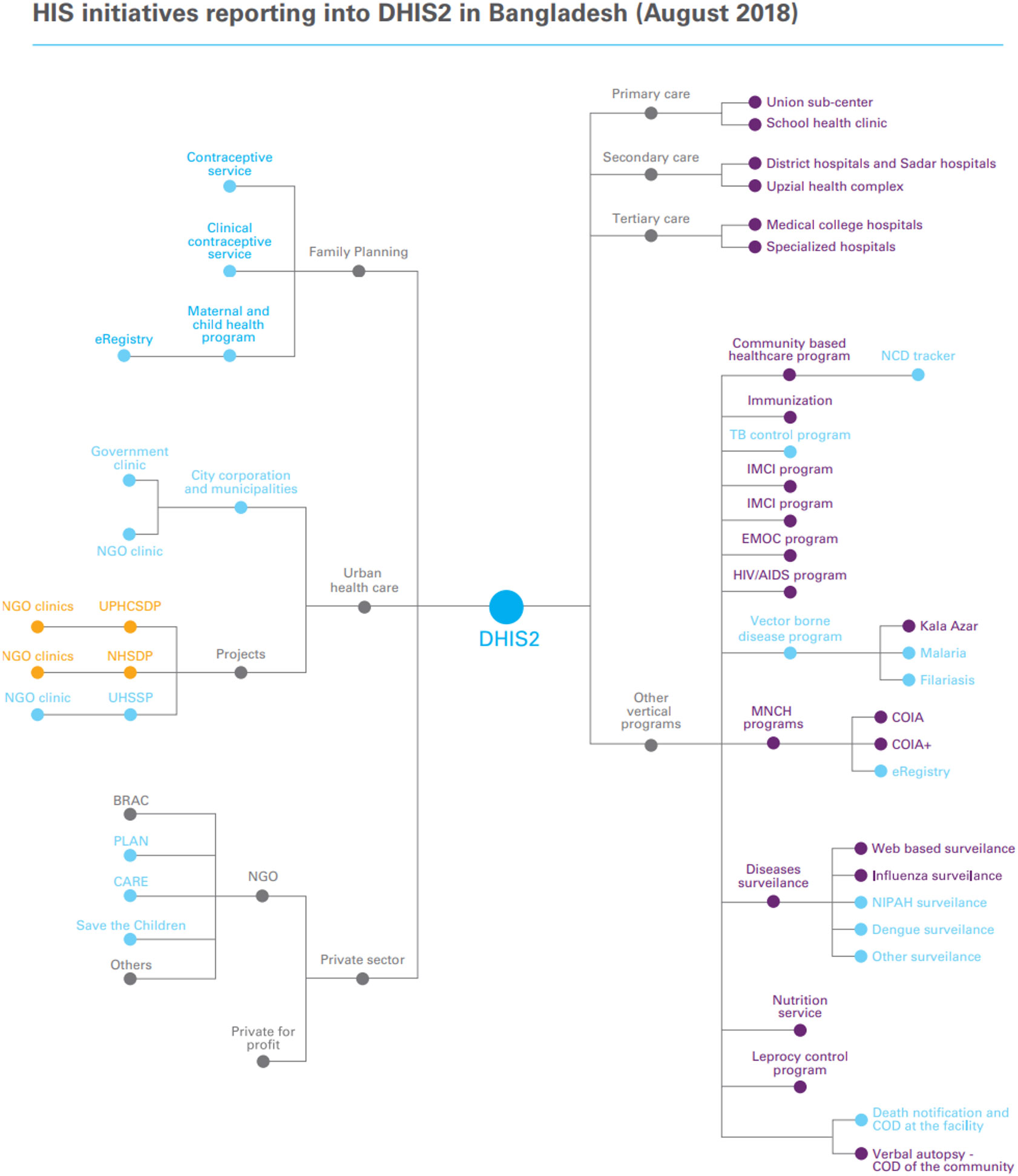
Source: Health System Strengthening: Transforming the health information system in Bangladesh through the implementation of DHIS2 (Case Study: Bangladesh, p. Kathmandu, Nepal). (2019). United Nations Children’s Fund Regional Office for South Asia.
The EPI falls under the Directorate General of Health Services, which operates upazila (sub-districts) health complexes, rural dispensaries, community clinics, and EPI outreach centers. Immunization data, including indicators reporting on the number of pregnant women receiving tetanus toxoid vaccine and the number of children under the age of five receiving scheduled vaccines by type, are collected at ward and union level clinics and facilities, submitted to the district level, aggregated, and then sent along up through the Division and finally to the national level (Figure 15).
Figure 15. Directorate General of Health Services Management Information System Data Flow
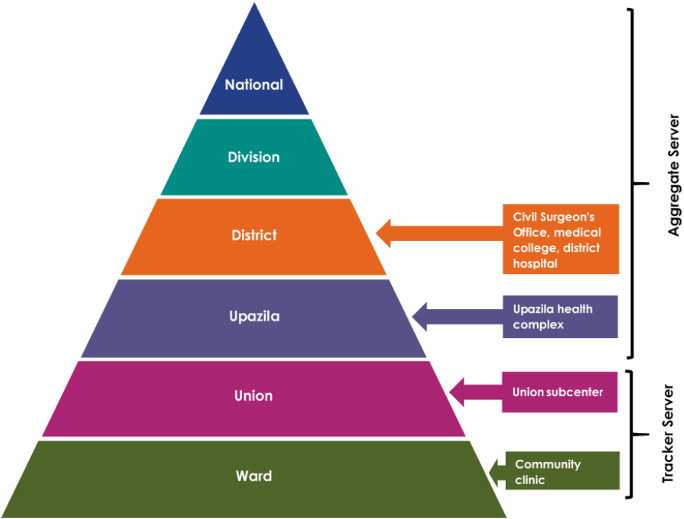
Source: Begum, Tahmina, Shaan Muberra Khan, Jannatul Ferdous, Muhammad Masud Parvez, Aminur Rahman, Feroza Akhter Kumkum, and Iqbal Anwar. 2019. “Using DHIS 2 Software to Collect Health Data in Bangladesh.” Working Paper. Data for Impact.
At the community level, where immunization services are commonly offered, more than 13,000 community clinics enter information into the system.41 One important feature of the system for immunization services is that health workers have access to individual records, which contain contact information. Using this contact information, health workers can follow up with families of children who may have missed immunizations.42
Bangladesh has introduced several initiatives to improve the quality of HMIS data, from data validation within the DHIS2 system to data quality self-assessments facilitated by UNICEF and WHO and trainings held with district and upazila managers to improve capacity for data collection and reporting.43 However, despite these efforts, concerns about the quality of data remain. One report from UNICEF suggested that the focus has historically been on reporting rates at the expense of data quality and utilization.44 Some of the documented barriers to data quality and use include limited human resources, frequent DHIS2 version changes, poor network connectivity, limited IT infrastructure, and resistance to convert from paper to an electronic system.45
Civil registration and vital statistics, which includes birth registration, are an important component of government systems in a country as they lay the groundwork for government planning and policy and promote access to essential services such as healthcare and education.46 For the purposes of immunization, accurate birth registration data is essential for identifying children born in a given year and for use as a denominator for many immunization coverage indicators. In Bangladesh, birth registration is legally mandated and collected as part of the online Birth and Death Registration Information System which is linked with the country’s HMIS. The system in Bangladesh is advanced in that it is fully electronic at all levels, but overall, birth registration coverage remains low with just over one in five births registered within one year.47
Documented data quality audits of immunization data in Bangladesh were not identified through the literature search. This may be an area for further investigation by the CLHs.
Community Health Structure and Role in Routine Immunization
The MoHFW employs three different cadre of community health workers, all of which work in community health clinics, including family welfare assistants (FWAs), health assistants (HAs), and community health care providers (CHCPs). These paid community health workers support health promotion, community mobilization, and provision for a range of services, including child health and immunization. NGOs operating in the country also employ their own cadres of community health workers, but these three positions are the only cadres employed by the MoHFW.48
Immunization Program Details
In Bangladesh, EPI is implemented through various outreach centers as well as clinic-based activities. The EPI service in rural areas depends on the systems of different districts, upazilas, wards, and blocks and sub-blocks (the administrative unit used in formal refugee camps). Each sub-block has an EPI outreach site where EPI services are provided to the population. The EPI program also provides motivational and educational awareness on immunization during household visits by health workers like HAs and FWAs. Immunization services are also available at outreach sites like EPI sites, satellite clinics, static clinics, and community clinics.49
Immunization services in Bangladesh are provided through a network of public, private, and NGO facilities. The government first partnered with NGOs in the 1980’s when it was intensifying its EPI programming to reach its goal of universal childhood immunization by 1990. NGOs have continued to play an important role in both supporting the EPI at national and sub-national levels through technical assistance, program management, monitoring, and community mobilization, and directly providing immunization services in some areas.50 This is particularly true in urban areas, where local governments contract with a network of NGOs to provide almost all immunizations.51 For example, national NGOs deliver more than 95 percent of immunization services in the city of Dhaka. The NGOs are accountable to the municipal government, which supports them in planning and monitoring, and to the MoHFW, which provides vaccine supplies and other logistical support.52 NGOs cover immunization services in approximately 58 percent of urban slum communities and 53 percent of non-slum communities across urban regions in Bangladesh.53 As per the National Immunization Policy, private sector facilities and providers who receive vaccines from the government to provide routine immunization services cannot charge clients for either the vaccine or service.54
Environmental Context
Climate Change
Bangladesh is no exception to the increasing risk that climate change poses to public health worldwide. Recent studies suggest that climate change is creating new challenges that require urgent attention and adaptation measures to ensure the continuity of vaccination programs and the decline in ZD children.55, 56 One of the ways that climate change is changing immunization efforts in Bangladesh is through interferences in the vaccine supply chain.57, 58 Changes in temperature, rainfall patterns, and extreme weather events can affect the storage and transportation of vaccines, potentially leading to reduced vaccine efficacy.59, 60 For example, during heatwaves or power outages, vaccines may not be stored at the optimal temperature, which can compromise their effectiveness. Similarly, heavy rains or floods can damage roads and infrastructure, making it difficult to transport vaccines to remote or hard-to-reach areas.
The El Niño-Southern Oscillation (ENSO) is a major driver of climate variability in Bangladesh, influencing the population dynamics of cholera.61 Warmer and drier conditions associated with ENSO can lead to outbreaks of cholera, a water-borne disease that can be prevented through vaccination. In addition, monsoon flooding is affecting the seasonality and transmission of rotavirus, a common cause of diarrhea in children.62 Higher humidity and temperature are also linked to increased incidence of typhoid or enteric fever in Bangladesh.63
Climate-related migration and displacement may also lead to gaps in immunization coverage.64 The effects of climate change, including flooding, drought, and other extreme weather events, can displace people from their homes. These people may have difficulty accessing routine health services, including vaccinations, which can result in gaps in immunization coverage and an increased risk of disease outbreaks. Moving forward, further study on the specific impacts of climate change on provision and accessibility of immunization services will be helpful to better understand the magnitude of the disruption and track changes over time.
Areas for Further Inquiry
While this landscape attempts to present a holistic picture of the immunization context in Bangladesh, information gaps remain that will be critical to fill in order to effectively and sustainably reach ZD and under-immunized children and missed communities, as shown in Table 4.
Table 4. Summary of the Gaps and Rationale for Additional Inquiry
| Gap | Rationale |
|---|---|
| Evidence regarding data quality of administrative data sources for accurately calculating immunization coverage and estimating populations | The data in this area are extremely limited. More information about data quality challenges could be used to craft solutions to promote the use of high-quality, hyper-local administrative data, which could be transformative in the identification and reach of ZD and under-immunized children. |
| Information about staffing levels for critical human resources supporting immunization services | Current data in this area are limited, particularly for remote and hard-to-reach areas. More information about staffing levels for the variety of cadre supporting immunization services could be used to identify current gaps, but also predict future gaps and inform human resource programming and advocacy efforts. |
| Immunization coverage data among historically marginalized populations | Current, detailed data focused on immunization coverage among ethnic minority groups, refugee communities, and remote and hard-to-reach communities are limited. Quantitative coverage data as well as in-depth, qualitative inquiry regarding barriers to immunization are important when developing context-specific strategies to reach ZD and under-immunized children. |
| Information about additional environmental factors that impact immunization coverage in the country | The current evidence on the direct effects of climate change on immunization are limited for Bangladesh, specifically. Additionally, other environmental factors, such as political will, conflict and insecurity, and trust in government are important contributors to immunization uptake that should be examined to help inform programming targeting ZD and under-immunized children. |
Immunization Partners and Zero Dose Efforts
Table 5 below shows a list of immunization stakeholders engaged in zero-dose efforts in Bangladesh. The content will be expanded in future iterations of the landscape through a series of planned key informant interviews with stakeholders at national and subnational levels.
Table 5. List of Preliminary Stakeholders in Immunization
| Sl. No. | Organization/Entity | Category | Geographic coverage | Dates of work | Funder | Description of work |
|---|---|---|---|---|---|---|
| 1 | United Nations International Children's Emergency Fund (UNICEF)- Bangladesh | Funder/Technical Assistance | International | 1952-present | UNICEF | To support the country’s efforts to respond to the most vulnerable children, including working with the district health administration to provide immunization services. |
| 2 | Centre for Health and Population Research, Bangladesh (icddr,b) | Research and Implementation | International | 1960-present | A combination of core support from bilateral donors and grant income, including Bill & Melinda Gates Foundation, USAID, and the United Nations Sustainable Development Group (UNSDG) | To conduct high-quality research that addresses health priorities and translates to policy and practice. |
| 3 | World Bank | Funder | International | 1971-present | The International Development Association (IDA) | To support Bangladesh’s development journey including poverty reduction and economic growth acceleration. |
| 4 | World Health Organization (WHO) | Funder/Technical Assistance | International | 1972-present | WHO | To provide technical advice and support to improve the health and development of Bangladeshis, including monitoring and assessing trends in health indicators. |
| 5 | National Polio and Measles-Rubella Laboratory (NPML), the Institute of Public Health | Research and Implementation | International | 1995-present | Global Polio Eradication Initiative (GPEI) & WHO | Supports polio laboratory diagnosis (and later, measles and rubella diagnosis). |
| 6 | Gavi | Funder | International | 2001-present | Gavi | Funds initiatives to promote vaccination of the children against deadly and debilitating infectious diseases. |
| 7 | BRAC James P Grant School of Public Health, BRAC University | Research and Implementation | International | 2004-present | BRAC, icddr,b and BRAC University | To create innovative public health leaders and solutions through cutting-edge, experiential education, training, research and advocacy. |
| 8 | National Committee for Immunization Practice (NCIP) | Government | International | 2008-2018 | WHO | They are multidisciplinary bodies of national experts that provide evidence-based recommendations to policymakers and immunization program managers. |
| 9 | National Immunization Technical Advisory Group (NITAG) | Government | International | 2019-present | WHO | |
| 10 | Bangladesh Medical Research Council (BMRC) | Research and Implementation | National | 1972-present | Ministry of Health and Family Welfare | An autonomous national research body that carries out research on medical and health sciences and plans and prioritize research in Bangladesh. |
| 11 | National Institute of Preventive and Social Medicine (NIPSOM) | Research and Implementation | National | 1974-present | Ministry of Health and Family Welfare | A national public health institute in Dhaka. |
| 12 | Institute of Epidemiology, Disease Control and Research (IEDCR) | Government | National | 1976- | Ministry of Health and Family Welfare | The Government of Bangladesh’s research institute, responsible for researching epidemiological and communicable disease in Bangladesh as well as disease control. |
| 13 | Immunization Platform of Civil Society in Bangladesh (IPCSB) | National | 2014-present | Ministry of Health and Family Welfare | Civil society NGO platform with an aim to strengthen health systems in Bangladesh to improve immunization in areas of low coverage through training of service providers, research, and advocacy. | |
| 14 | National Institute of Population Research and Training (NIPORT) | Government | National | Ministry of Health and Family Welfare | To provide task-oriented in-service training to health and family planning personnel and conduct operations research to ensure efficacy and efficiency of health services. |
Relevant Resources
Below are several relevant resources related to health and immunization in Bangladesh, including surveys, data, reports, and databases.
Surveys
Immunization and Health Data
Program Reports, National Strategies and Databases
- National Immunization Strategy (NIS) 2023-2027 for Expanded Program on Immunization (EPI) of Bangladesh
- Bangladesh Comprehensive Multi-Year Plan for Immunization 2018-2022
- WHO EPI 2020 Factsheet for Bangladesh
- Report on Bangladesh Sample Vital Statistics 2018
- Bangladesh 8th Five Year Plan: July 2020-June 2025
- Global Health Expenditure Database- 2022 Release
Anticipated Work/Publications
- Bangladesh Demographic and Health Survey – 2022
References
1 Carter, Austin, William Msemburi, So Yoon Sim, Katy A. M. Gaythorpe, Ann Lindstrand, and Raymond C. W.Hutubessy. 2021. “Modeling the Impact of Vaccination for the Immunization Agenda 2030: Deaths Averted Due to Vaccination Against 14 Pathogens in 194 Countries from 2021-2030.” SSRN ScholarlyPaper. Rochester, NY.
2 Wendt, Andrea, Thiago M. Santos, Bianca O. Cata-Preta, Luisa Arroyave, Daniel R. Hogan, Tewodaj Mengistu, Aluisio J. D. Barros, and Cesar G. Victora. 2022. “Exposure of Zero-Dose Children to Multiple Deprivation: Analyses of Data from 80 Low- and Middle-Income Countries.” Vaccines 10 (9): 1568.
3 United Nations, Department of Economic and Social Affairs, Population Division. 2022. “World Population Prospects 2022, Online Edition.”
4 “Levels & Trends in Child Mortality: Report 2022.” 2023. Estimates Developed by the United Nations Inter-Agency Group for Child Mortality Estimation. United Nations Children’s Fund, World Health Organization, World Bank Group, United Nations.
5 Bangladesh Bureau of Statistics. 2019. “Report on Bangladesh Sample Vital Statistics 2018.” Bangladesh: Ministry of Planning, Statistics and Informatics Division.
6 Gavi Secretariat. 2023. “Bangladesh Zero Dose Analysis.” Unpublished.
7 Ibid.
8 Ibid.
9 Government of People’s Republic of Bangladesh. 2022. “National Immunization Strategy (NIS) 2023-2027 for Expanded Program on Immunization (EPI) of Bangladesh.”
10 Burton, Anthony. 2009. “WHO and UNICEF Estimates of National Infant Immunization Coverage: Methods and Processes.” Bulletin of the World Health Organization 87 (7): 535–41.
11 Gavi Secretariat. 2023. “Bangladesh Zero Dose Analysis.” Unpublished.
12 Hanifi, Sayed Manzoor Ahmed, Nujhat Jahan, Nazia Sultana, Sharif-Al Hasan, Ashish Paul, and Daniel D. Reidpath. 2022. “Millions of Bangladeshi Children Missed Their Scheduled Vaccination Amidst COVID-19 Pandemic.” Frontiers in Public Health 9 (January): 738623.
13 Rana, Shohel, Rashed Shah, Sabbir Ahmed, and Golam Mothabbir. 2021. “Post-Disruption Catch-up of Child Immunisation and Health-Care Services in Bangladesh.” The Lancet Infectious Diseases 21 (7): 913.
14 Hanifi, Sayed Manzoor Ahmed, Nujhat Jahan, Nazia Sultana, Sharif-Al Hasan, Ashish Paul, and Daniel D. Reidpath. 2022. “Millions of Bangladeshi Children Missed Their Scheduled Vaccination Amidst COVID-19 Pandemic.” Frontiers in Public Health 9 (January): 738623.
15 Angeles, Gustavo, Hannah Silverstein, Kara Zunaid Ahsan, Mohammad Kibria, Nibras Ar Rakib, and Gabriela Escudero. 2021. “Estimating the Effects of COVID-19 on Immunization Services Use in Bangladesh.” Data for Impact, United States Agency for International Development.
16 Government of People’s Republic of Bangladesh. 2022. “National Immunization Strategy (NIS) 2023-2027 for Expanded Program on Immunization (EPI) of Bangladesh.”
17 Basnet, Sulochana, Edward A. Frongillo, Phuong Hong Nguyen, Spencer Moore, and Mandana Arabi. 2020. “Associations of Maternal Resources with Care Behaviours Differ by Resource and Behaviour.” Maternal & Child Nutrition 16 (3): e12977.
18 Kachoria, Aparna G., Mohammad Yousuf Mubarak, Awnish K. Singh, Rachael Somers, Saleh Shah, and Abram L. Wagner. 2022. “The Association of Religion with Maternal and Child Health Outcomes in South Asian Countries.” PLOS ONE 17 (7): e0271165.
19 Srivastava, Shobhit, T. Muhammad, Rashmi Rashmi, and Pradeep Kumar. 2022. “Socioeconomic Inequalities in Non- Coverage of Full Vaccination among Children in Bangladesh: A Comparative Study of Demographic and Health Surveys, 2007 and 2017–18.” BMC Public Health 22 (1): 183.
20 Basnet, Sulochana, Edward A. Frongillo, Phuong Hong Nguyen, Spencer Moore, and Mandana Arabi. 2020. “Associations of Maternal Resources with Care Behaviours Differ by Resource and Behaviour.” Maternal & Child Nutrition 16 (3): e12977.
21 Kachoria, Aparna G., Mohammad Yousuf Mubarak, Awnish K. Singh, Rachael Somers, Saleh Shah, and Abram L. Wagner. 2022. “The Association of Religion with Maternal and Child Health Outcomes in South Asian Countries.” PLOS ONE 17 (7): e0271165.
22 Boulton, Matthew L., Bradley F. Carlson, Laura E. Power, and Abram L. Wagner. 2018. “Socioeconomic Factors Associated with Full Childhood Vaccination in Bangladesh, 2014.” International Journal of Infectious Diseases 69 (April): 35–40.
23 Uddin, Md Jasim, Charles P. Larson, Elizabeth Oliveras, A. I. Khan, M. A. Quaiyum, and Nirod Chandra Saha. 2010. “Child Immunization Coverage in Urban Slums of Bangladesh: Impact of an Intervention Package.” Health Policy and Planning 25 (1): 50–60.
24 Feldstein, Leora R., Sarah D. Bennett, Concepcion F. Estivariz, Gretchen M. Cooley, Lauren Weil, Mallick Masum Billah, M. Salim Uzzaman, et al. 2020. “Vaccination Coverage Survey and Seroprevalence among Forcibly Displaced Rohingya Children, Cox’s Bazar, Bangladesh, 2018: A Cross-Sectional Study.” PLoS Medicine 17 (3): e1003071.
25 Ahmed, Nawshin, A. S. M. Ishtiak, Md Faisal Kabir Rozars, Atia Sharmin Bonna, K. M. Pritam Alam, Md Elias Hossan, Rajib Das, et al. 2023. “Factors Associated with Low Childhood Immunization Coverage among Rohingya Refugee Parents in Cox’s Bazar, Bangladesh.” PLOS ONE 18 (4): e0283881.
26 Jalloh, Mohamed F., Sarah D. Bennett, Didarul Alam, Paryss Kouta, Dalia Lourenço, Mohammad Alamgir, Leora R. Feldstein, et al. 2019. “Rapid Behavioral Assessment of Barriers and Opportunities to Improve Vaccination Coverage among Displaced Rohingyas in Bangladesh, January 2018.” Vaccine 37 (6): 833–38.
27 World Health Organization. 2022. “Global Health Expenditure Database- 2022 Release.” January 24, 2022.
28 Arsenault, Catherine, Mira Johri, Arijit Nandi, José M. Mendoza Rodríguez, Peter M. Hansen, and Sam Harper. 2017. “Country-Level Predictors of Vaccination Coverage and Inequalities in Gavi-Supported Countries.” Vaccine 35 (18): 2479–88.
29 Wagstaff, Adam, Patrick Eozenou, and Marc Smitz. 2019. “Out-of-Pocket Expenditures on Health,” April.
30 World Health Organization. 2021. “Global Expenditure on Health: Public Spending on the Rise?” Global Report.
31 Sim, So Yoon, Elizabeth Watts, Dagna Constenla, Logan Brenzel, and Bryan N. Patenaude. 2020. “Return On Investment From Immunization Against 10 Pathogens In 94 Low- And Middle-Income Countries, 2011–30.” Health Affairs 39 (8): 1343–53.
32 World Health Organization. 2022. “Global Health Expenditure Database- 2022 Release.” January 24, 2022.
33 Uddin, Jasim, Haribondhu Sarma, Tajul I. Bari, and Tracey P. Koehlmoos. 2013. “Introduction of New Vaccines: Decision-Making Process in Bangladesh.” Journal of Health, Population, and Nutrition 31 (2): 211–17.
34 Government of People’s Republic of Bangladesh. 2022. “National Immunization Strategy (NIS) 2023-2027 for Expanded Program on Immunization (EPI) of Bangladesh.”
35 General Economics Division, Bangladesh Planning Commission. 2020. “8th Five Year Plan: July 2020-June 2025.” Dhaka, Bangladesh: Government of the People’s Republic of Bangladesh.
36 World Health Organization. 2022. “National Health Workforce Accounts (NHWA) Data Platform.” December 2022.
37 “Comprehensive Multi-Year Plan 2018-2022 for National Immunization Program of Bangladesh.” 2017. Government of People’s Republic of Bangladesh.
38 “Comprehensive Multi-Year Plan 2018-2022 for National Immunization Program of Bangladesh.” 2017. Government of People’s Republic of Bangladesh.
39 Government of People’s Republic of Bangladesh. 2022. “National Immunization Strategy (NIS) 2023-2027 for Expanded Program on Immunization (EPI) of Bangladesh.”
40 “Health System Strengthening: Transforming the Health Information System in Bangladesh through the Implementation of DHIS2.” 2019. Case Study: Bangladesh. United Nations Children’s Fund Regional Office for South Asia.
41 Begum, Tahmina, Shaan Muberra Khan, Jannatul Ferdous, Muhammad Masud Parvez, Aminur Rahman, Feroza Akhter Kumkum, and Iqbal Anwar. 2019. “Using DHIS 2 Software to Collect Health Data in Bangladesh.” Working Paper. Data for Impact.
42 “Health System Strengthening: Transforming the Health Information System in Bangladesh through the Implementation of DHIS2.” 2019. Case Study: Bangladesh. United Nations Children’s Fund Regional Office for South Asia.
43 Government of People’s Republic of Bangladesh. 2022. “National Immunization Strategy (NIS) 2023-2027 for Expanded Program on Immunization (EPI) of Bangladesh.”
44 “Health System Strengthening: Transforming the Health Information System in Bangladesh through the Implementation of DHIS2.” 2019. Case Study: Bangladesh. United Nations Children’s Fund Regional Office for South Asia.
45 Begum, Tahmina, Shaan Muberra Khan, Jannatul Ferdous, Muhammad Masud Parvez, Aminur Rahman, Feroza Akhter Kumkum, and Iqbal Anwar. 2019. “Using DHIS 2 Software to Collect Health Data in Bangladesh.” Working Paper. Data for Impact.
46 Rahman, M. Hafizur, Amber Bickford Cox, and Samuel L. Mills. 2019. “A Missed Opportunity: Birth Registration Coverage Is Lagging behind Bacillus Calmette–Guérin (BCG) Immunization Coverage and Maternal Health Services Utilization in Low- and Lower Middle-Income Countries.” Journal of Health, Population, and Nutrition 38 (Suppl 1): 25.
47 Chong, Serena. 2022. “Assessing Partner Alignment in Support of the Health Information System in Bangladesh.” Health Data Collaborative, UNICEF.
48 Egan, Kimberly Farnham, Kristen Devlin, and Tanvi Pandit Rajani. 2017. “Community Health Systems Catalog Country Profile: Bangladesh.” Arlington, VA: USAID Advancing Partners & Communities.
49 Sarkar, Probir Kumar, Nital kumar Sarker, Sharmim Doulah, and Tajul Islam A. Bari. 2015. “Expanded Programme on Immunization in Bangladesh: A Success Story.” Bangladesh Journal of Child Health 39 (2): 93–98.
50 Arifeen, Shams El, Aliki Christou, Laura Reichenbach, Ferdous Arfina Osman, Kishwar Azad, Khaled Shamsul Islam, Faruque Ahmed, Henry B. Perry, and David H. Peters. 2013. “Community-Based Approaches and Partnerships: Innovations in Health-Service Delivery in Bangladesh.” The Lancet 382 (9909): 2012–26.
51 “Comprehensive Multi-Year Plan 2018-2022 for National Immunization Program of Bangladesh.” 2017. Government of People’s Republic of Bangladesh.
52 Uddin, Md Jasim, Charles P Larson, Elizabeth Oliveras, A I Khan, M A Quaiyum, and Nirod Chandra Saha. 2010. “Child Immunization Coverage in Urban Slums of Bangladesh: Impact of an Intervention Package.” Health Policy and Planning 25 (1): 50–60.
53 “Comprehensive Multi-Year Plan 2018-2022 for National Immunization Program of Bangladesh.” 2017. Government of People’s Republic of Bangladesh.
54 Directorate General of Health Services, Ministry of Health and Family Welfare. 2013. “National Immunization Policy.”
55 Nahian, Mahin Al. 2023. “Public Health Impact and Health System Preparedness within a Changing Climate in Bangladesh: A Scoping Review.” Challenges 14 (1): 4.
56 Hasib, Enamul, and Prita Chathoth. 2016. “Health Impact of Climate Change in Bangladesh: A Summary.” Current Urban Studies 04 (01): 1–8.
57 Directorate General of Health Services, Ministry of Health and Family Welfare, Government of the People’s Republic of Bangladesh. 2018. “Bangladesh Health-National Adaptation Plan (HNAP).” World Health Organization Bangladesh, Institute of Epidemiology, Disease Control & Research.
58 Mahmud, Ayesha S., Pamela P. Martinez, Jingxing He, and Rachel E. Baker. 2020. “The Impact of Climate Change on Vaccine-Preventable Diseases: Insights From Current Research and New Directions.” Current Environmental Health Reports 7 (4): 384–91.
59 Directorate General of Health Services, Ministry of Health and Family Welfare, Government of the People’s Republic of Bangladesh. 2018. “Bangladesh Health-National Adaptation Plan (HNAP).” World Health Organization Bangladesh, Institute of Epidemiology, Disease Control & Research.
60 Mahmud, Ayesha S., Pamela P. Martinez, Jingxing He, and Rachel E. Baker. 2020. “The Impact of Climate Change on Vaccine-Preventable Diseases: Insights From Current Research and New Directions.” Current Environmental Health Reports 7 (4): 384–91.
61 Mahmud, Ayesha S., Pamela P. Martinez, Jingxing He, and Rachel E. Baker. 2020. “The Impact of Climate Change on Vaccine-Preventable Diseases: Insights From Current Research and New Directions.” Current Environmental Health Reports 7 (4): 384–91.
62 Ibid.
63 Ibid.
64 Nayna Schwerdtle, Patricia, Kate Baernighausen, Sayeda Karim, Tauheed Syed Raihan, Samiya Selim, Till Baernighausen, and Ina Danquah. 2021. “A Risk Exchange: Health and Mobility in the Context of Climate and Environmental Change in Bangladesh-A Qualitative Study.” International Journal of Environmental Research and Public Health 18 (5): 2629.