Mali Zero-Dose Landscape

Background
The Gavi Zero-Dose Learning Hub (ZDLH) is responsible for highlighting work and outputs generated by the four Gavi Country Learning Hubs (CLHs) in Bangladesh, Mali, Nigeria, and Uganda with the objective of using this evidence to better understand the factors influencing implementation and performance of approaches to identify and reach zero-dose (ZD) and under-immunized children as well as missed communities. The consortium, led by JSI in partnership with the Indian Institute of Health Management Research (IIHMR) and the Geneva Learning Foundation (TGLF), aims to support CLHs to implement the identification, reach, monitoring, measurement, and advocacy (IRMMA) framework, facilitate sharing and learning across the CLHs, contribute evidence to capture, synthesize and disseminate the breadth of learning across the Alliance, and ultimately to help improve immunization equity and reduce the number of ZD and under-immunized children globally by facilitating quality evidence generation and uptake.
In pursuit of these objectives, the ZDLH has developed ZD landscapes to synthesize the evidence to date on immunization prevalence, policy, and programming related to ZD and under-immunized children in each of the four learning hub countries. These ZD landscape analyses describe the current immunization and ZD context, including coverage trends, equity, health systems, and existing partners and programming to orient implementers and funders to the broad immunization context and opportunities for intervention to reduce the prevalence of ZD children. While the ZD landscapes synthesize the existing literature and data, the CLHs in Mali and other countries will generate new evidence based on their own country-level ZD programming and activities such as rapid assessments and surveys.
The purpose of this landscape is to provide the Gavi CLH and stakeholders in Mali with a comprehensive overview of the immunization landscape within the country, with a special focus on ZD and under-immunized children. Operationally, Gavi defines a ZD child as one who has not received a single dose of a diphtheria, tetanus, and pertussis-containing vaccine. Given the highly variable and contextual nature of the drivers, barriers, and programmatic approaches to reach ZD and under-immunized children, it is important to understand the unique context, policies, and economics of the country. This will not only help guide approaches, but also to better understand and interpret why changes in IRMMA may or may not occur. This landscape also aims to inform research and programming efforts in Mali by identifying important knowledge gaps related to the identification, reach, monitoring, measurement, and advocacy for ZD and under-immunized children.
Methods
The Mali ZD landscape assessment is based on a review of existing literature and secondary analysis of existing data from recent national surveys and global immunization databases. To identify relevant literature, the ZDLH team searched both gray and peer-reviewed sources, ministry and partner websites, and existing Gavi reviews and resources. Domains of interest included immunization coverage and equity as well as information about the health system in which the immunization program operates, including, but not limited to, human resources, financing, immunization policies, and the health system structure. Relevant publications were identified and reviewed and information related to the ZD or immunization context in each country was extracted. Where gaps in information remain, the team relied on input from members of the Mali CLH and may conduct additional key informant interviews (KIIs) as part of the complementary political economy analysis (PEA). This landscape is intended to represent the current situation in the learning hub countries, and therefore will be updated on an annual basis to include new resources including those generated by the CLHs.
Introduction
Childhood vaccination rates in Mali have increased nearly 20 percent since 2001, paired with a nearly 50 percent decrease in the under-five mortality rate.1 Even greater strides have been made in the reduction of under-five mortality by diphtheria, measles, and tetanus, with decreases of more than 75 percent since 2001.2 Despite these strides, fewer than half of Malian children have received all essential childhood vaccines.3 Immunization coverage varies widely from region to region due in part to regional conflicts disrupting parts of the health system, including routine vaccination for children.4 Under- and un-immunized children in areas affected by conflict as well as displaced children and those in communities that are nomadic by nature are particularly challenging to reach. Identifying approaches to tracking and reaching these children is critical to reaching full and equitable immunization coverage in Mali.
Mali is a landlocked country located in West Africa that shares its borders with seven nations (Figure 1). As of 2022, Mali has an estimated population of over 22 million people, of which approximately 4.1 million are children under five (Table 1).5
Figure 1. Map of Mali

Table 1. Total Population and Residence
| Total Population (2022) | |
|---|---|
| Total | 22,593,591 |
| Male | 11,406,820 (50.5%) |
| Female | 11,186,771 (49.5%) |
| Residence (2022) | |
|---|---|
| Rural | 55.3% |
| Urban | 44.7% |
Source: United Nations, Department of Economic and Social Affairs, Population Division. World Population Prospects, 2022.
As noted previously, Mali has achieved a nearly 50 percent decrease in mortality among children under five since 2000 (Figure 2). However, the United Nations Inter-agency Group for Child Mortality Estimation (UN IGME) estimates that approximately 85,000 children died in 2021 from a variety of causes, including from vaccine-preventable diseases.6
Source: United Nations Inter-agency Group for Child Mortality Estimation (2023).
The 2019 Global Burden of Disease study found that nearly 20 percent of deaths among children under five in Mali may have been the result of vaccine-preventable illnesses, including meningitis, measles, and some lower respiratory infections (Figure 3).
Source: Institute for Health Metrics and Evaluation (IHME). GBD Results, Mali. Seattle, WA: IHME, University of Washington, 2020.
Improved access to immunization is a principal driver of the decrease in under-five mortality in developing countries.7 Three decades of routine immunization programs have contributed to dramatic declines in vaccine-preventable diseases such as measles in countries like Mali (Figure 4). Mali’s recent application (July 2023) to Gavi for support in rolling out the malaria vaccine may result in an even greater reduction in vaccine-preventable death in the country.8
Source: IHME. GBD Results, Mali. Seattle, WA: IHME, University of Washington, 2020. Available from https://vizhub.healthdata.org/gbd-results/.); ICF, 2015. The DHS Program STATcompiler. Funded by USAID.
Immunization Context
Despite increases in vaccination coverage over time, gaps in immunization continue to contribute to under-five morbidity and mortality in Mali. One 2021 study found that 14 percent of pneumonia cases among Malian children in the study population were attributable to vaccine-preventable diseases, despite a pentavalent vaccine coverage rate of approximately 75 percent.9 ZD children are estimated by Gavi to represent 25 percent of all deaths (18,529 total deaths) among children under five in the country.10
Immunization Schedule
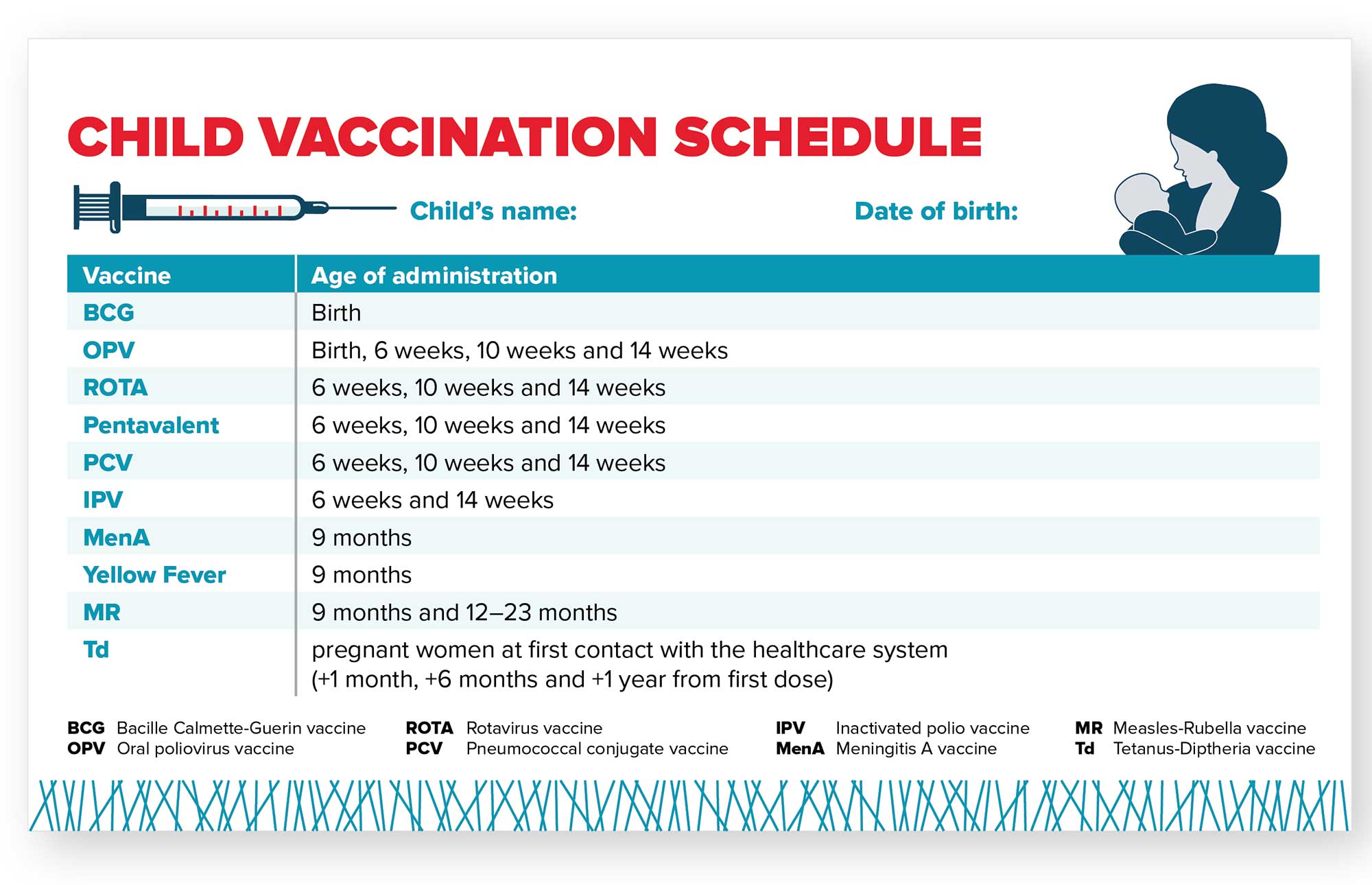
Mali’s immunization schedule includes 10 different vaccines and targets approximately 900,000 children each year. Mali administers the pentavalent vaccine, which prevents diphtheria, tetanus, pertussis, hepatitis B, and Haemophilus influenzae type b (Hib) (Figure 5).
Figure 5. Mali Childhood Vaccination Schedule
Coverage Estimates
Mali’s current coverage estimates for six basic immunizations range from 83 percent of children receiving the Bacille Calmette-Guerin (BCG) vaccine at birth to 33 percent of children receiving the second dose of the measles-containing vaccine (MCV) at 12-23 months of age (Figure 6). Mali could prevent an estimated 238,000 future deaths through currently forecasted preventive immunization activities between 2021-2025.11
Source: World Health Organization/UNICEF Estimates of National Immunization Coverage (WUENIC)—2021 estimates. (2022). WHO Immunization Data Portal.
Identifying and reaching ZD and under-immunized children in Mali is essential to meeting the Gavi 5.0 equity goal and to progress toward reaching all eligible children with routine vaccination in the country. Estimating the number of ZD children in Mali requires estimates of Penta1 coverage and the total number of surviving children. These estimates can vary based on the source of the data, resulting in different estimates of the population of ZD children (Table 2). Positive estimates (those above zero) range from 157,055 (from the World Health Organization [WHO]/United Nations Children’s Fund [UNICEF] Estimates of National Immunization Coverage [WUENIC]) to 210,319 ZD children (from the Institute for Health Metrics and Evaluation [IHME]).12
Table 2. Mali ZD Estimate Inputs
| Source | Total Number of Surviving Infants | Penta 1 Coverage | Number of ZD Children |
|---|---|---|---|
| WUENIC (2021) | 872,528 | 82% | 157,055 |
| IHME (2020) | 876,328 | 76% | 210,319 |
Source: Gavi Secretariat. 2022. “Mali Zero Dose Analysis.” Unpublished
National administrative data from 2021 estimate Penta1 coverage at above 100 percent, resulting in a negative number of ZD children. However, the quality of administrative data can be problematic, evidenced by coverage rates of over 100 percent, which indicates an error in the documentation of the number of children receiving Penta1 vaccines or in the estimates of the total number of children.13
The goal of WUENIC analyses is to provide national immunization estimates on an annual basis. WUENIC immunization estimates are developed by triangulating data from several sources including government data, published and unpublished survey data, and consultation with local experts and governments. Statistical and mathematical modeling are not used to derive the final coverage estimates and estimates are not available at the sub-national level. As such, WUENIC estimates are not useful for identifying the location of ZD children in the country, but are useful for looking at trends in the ZD population over time.
IHME projections include different inputs and analyses because the goal of these estimates is different from those of WUENIC or administrative data. The goal of IHME is to generate highly-specific geospatial estimates of immunization coverage that are combined with additional data to generate national coverage estimates. IHME, like WUENIC, uses household survey data as well as national data, but it also uses covariates of immunization (such as residence or mother’s level of education) when calculating estimates. Using this data, IHME models immunization coverage at a hyper-local level (a five-by-five kilometer [km] area) and then incorporates additional higher-level data to model a national estimate.14 The resulting estimates provide more insight into the probable locations of ZD children within a country, but also include more assumptions and potential error than estimates generated from household surveys or administrative data. Given the differences in source data and estimation approaches, the true number (and location) of ZD children is not known. However, by triangulating the various estimates, we can determine where there is overlap and generate an informed estimate that can be used for broad planning purposes. Tailored implementation strategies to vaccinate ZD children may require other methods to better understand where they are located, how to reach them, and how to effectively bring them into routine immunization services.
For the purposes of this landscape, we will use data from both WUENIC and IHME sources with the understanding that the estimates are imperfect. Data from household surveys, like the Mali Demographic and Health Surveys (DHS), will also be incorporated into this assessment, particularly for equity analyses.
Effects of the COVID-19 Pandemic
After detecting its first case of COVID-19 in March 2020, Mali adopted measures to prevent disease spread, including restrictions on travel, bans on large public gatherings, and school closures.15 Maternal and child health service utilization, including immunization, dropped in the months following the onset of the pandemic.16 A study from Shapira et al. estimates that the number of children who received the third dose of the pentavalent vaccine decreased 17 percent between March and July 2020, with similar decreases in estimated measles and BCG coverage.17 Despite reinstating immunization services in the months following March 2020, one study estimates that by December 2020, vaccine service utilization had not yet reached pre-pandemic levels.18
Pandemic-related disruptions to immunization services were further exacerbated by security issues related to a military coup in 2020.19 A study from Amouzou et al. found that immunization service utilization disruptions were more significant in the areas affected by security issues.20 Additionally, rural districts of Mali faced greater declines in immunization coverage. Finally, Mali’s poverty rate rose by an estimated five percentage points in 2020, creating further challenges to immunization coverage.21
Equity
Gavi’s 5.0 strategy to identify and reach ZD and under-immunized children focuses on equity. To comprehensively implement Gavi’s 5.0 strategy, it is essential to examine the contexts in which ZD and under-immunized children live.
Factors Influencing ZD Status
Figure 7 presents sociodemographic characteristics for children who did not receive the Penta1, BCG, and measles vaccines. These three antigens, given at different times and different locations, can represent different immunization access barriers. Penta1 is typically used as a proxy indicator of access to routine immunization because it is given during well-child visits at 6, 10, and 14 weeks.
The measles vaccine, however, is given first at nine months and then again at 12-23 months at community-level health facilities, which also represents access to routine immunization services, albeit at a later age. BCG is given at birth in Mali, so its coverage may better represent birth in a health facility than access to routine immunization services.
Source: Mali Demographic and Health Survey 2018. Bamako, Mali, and Rockville, Maryland, USA: INSTAT and ICF.
The data presented in Figure 7, in addition to existing literature, indicate that household wealth, the mother’s education, and where a child lives are significant predictors of whether or not a child will receive measles, BCG, or Penta1 vaccination in Mali. Children of mothers who have a secondary or higher education are several times less likely to be ZD children than those whose mothers have received no education or only a primary level education. Additionally, children from poorer households are more likely to be ZD than children in households from the highest wealth quintiles.22
A child’s geographic location is an important predictor of ZD status in Mali. Children from rural areas are more than twice as likely to be ZD than children from urban areas. Notably, Mali is among the ten nations worldwide that have the largest gap in ZD children between urban and rural locations.23 Less populated northern regions of the country such as Kidal, Gao, and Tomboctou have a greater proportion of ZD children (ranging from 27.9 percent to 92.6 percent) compared with children in Bamako (6.7 percent). The Kidal region has a particularly high ZD prevalence, with nearly 93 percent of children not having received vaccination compared with Gao, which has the second highest proportion of ZD children (43.3 percent).
Data from the IHME (2021) suggest that while northern regions of the country have the highest prevalence of ZD children, the highest overall numbers can be found in the more heavily populated southern regions of the country, particularly in districts in the Bamako and Kayes regions (Figure 8). According to IHME estimates, nearly half of ZD children nationwide live in just 21 percent of districts, which are outlined in black in Figure 8 below. In addition to disparities in ZD status between geographic locations, disparities exist between ethnicities in Mali. Of the eight major ethnic groups in the country, the Touareg/Bella group has the highest proportion of ZD children (51.7 percent) followed by the Sonraï group (29.8 percent). Children in the Sarakole/Soninke/Marke ethnic groups are least likely to be ZD, with a ZD prevalence of 8.2 percent.24
Figure 8. Number of ZD Children by District
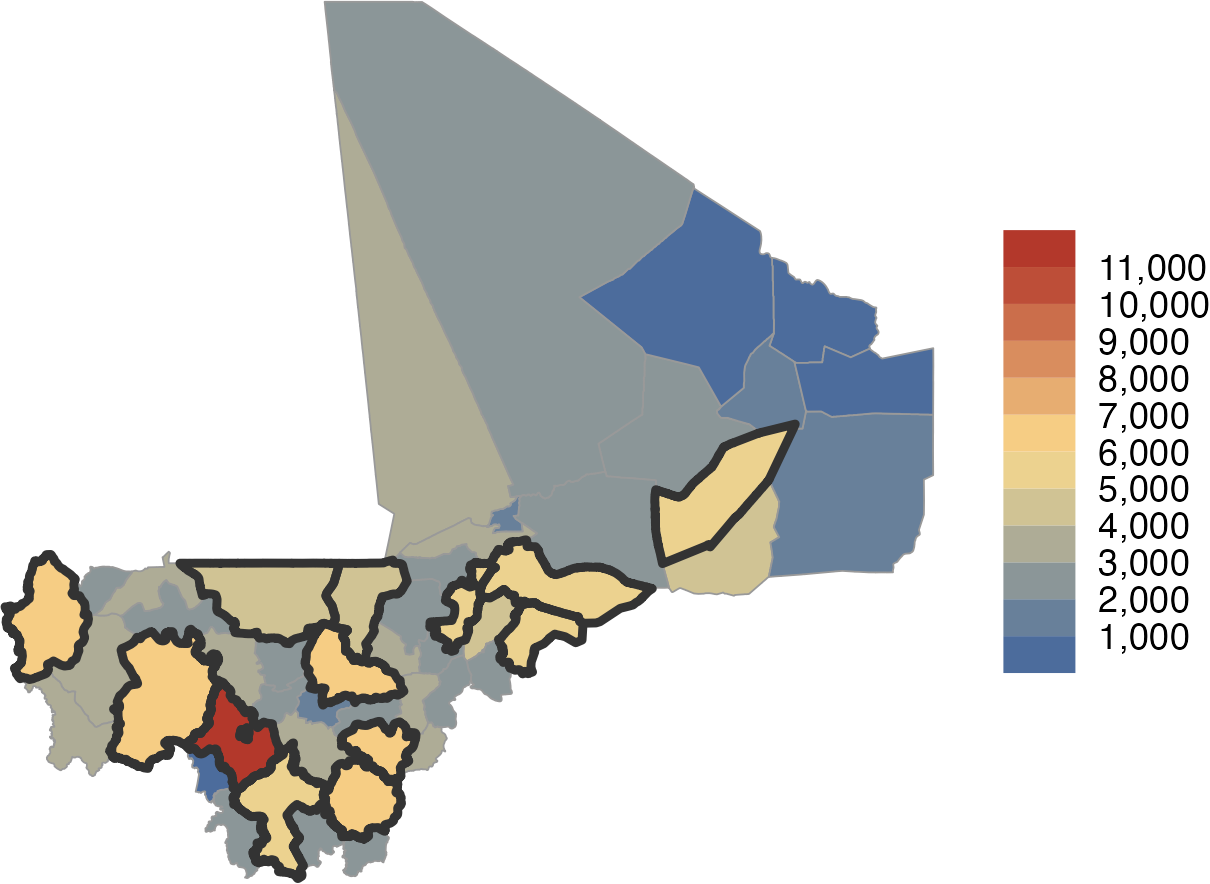
Source: IHME 2021 data cited in Gavi Secretariat, 2023. “Mali Zero Dose Analysis.” Unpublished.
A rise in conflict in the northern regions of Mali in 2012 created ongoing challenges in delivering essential health services, further exacerbating gaps in immunization coverage. A 2020 study examined maternal and child health indicators in the northern conflict regions of Mali compared to non-conflict regions. The analysis indicated that the prevalence of children in conflict regions aged 12 to 23 months who have received the Penta 3 vaccine dropped from more than 60 percent in 2010 to less than 40 percent in 2012 compared with more than 75 percent of children in non-conflict regions. While pentavalent coverage increased in both conflict and non-conflict regions between 2012 and 2018, a nearly 20 percent gap between conflict and non-conflict regions remains.25 A 2015 study of one refugee camp in northern Mali examined the impact of armed conflict on maternal and child health services. Qualitative findings indicated that mothers had little access to adequately resourced health facilities and that the conflict led to an uptick in home deliveries and the use of traditional medicines in response to childhood illnesses.26
Studies of ZD children among families that migrated to more southern regions of Mali as a result of conflict, as well as the impact of this migration on immunization systems, are largely absent from the literature. Additionally, comprehensive studies of vaccine hesitancy, the use of traditional medicine, and vaccination uptake among ethnic minorities are notable gaps in the available ZD research in Mali.
Health Systems
Mali has a decentralized healthcare system made up of the public and private sectors in addition to partner non-governmental organizations (NGOs) and donors.27 As shown in Figure 9, overall spending on healthcare as well as government spending on healthcare increased between 2005 and 2020 from 25 dollars per capita in 2005 to 35 dollars per capita in 2020. While healthcare spending has increased, the percentage of GDP spent on healthcare has remained largely steady at between four and five percent.28
Source: WHO Global Health Expenditure Database. Health Expenditure Profile, Mali.
Mali is among the countries with the lowest health expenditure per capita in the West Africa region, spending only modestly more than Niger (Figure 10). Mali is also among countries worldwide with the lowest health expenditure per capita, ranking 253 out of 286 countries in 2019.
Source: WHO Global Health Expenditure Database. Health Expenditure Profiles.
However, a better predictor of high immunization coverage is the combination of higher levels of government spending as a proportion of total spending on healthcare and low out-of-pocket spending.29 This is because greater government investment in programs like routine immunization and lower out-of-pocket costs for immunization make it more accessible to children from the poorest households and their families.30 Over the past 20 years, out-of-pocket spending as a proportion of total spending in Mali has decreased from 68.8 percent in 2000 to 28.7 percent in 2020. During that same time period, government spending on healthcare as a proportion of total healthcare spending increased from 23.7 percent to 34.4 percent (Figure 11). Both metrics combined indicate that Mali has made significant strides in immunization accessibility over the past 20 years.
Source: World Health Organization. 2022. “Global Health Expenditure Database- 2022 Release.” January 24, 2022.
Immunization Financing
Immunization is one of the most important and cost-effective public health interventions. According to one study, for every United States (U.S.) $1 spent on immunization between 2011 and 2020, there was an average return of up to 26 USD across a child’s lifetime.31 In 2022, Mali spent approximately 16 million USD on vaccines and routine immunization services, of which 11 percent was financed by the government and 89 percent was financed by external funders.32
Donor Support
Mali is currently one of 28 countries in the “initial self-financing” phase of eligibility for Gavi support, making the country eligible to apply for new vaccine support or health system and immunization strengthening.33 Gavi is the largest source of external financing for immunization in Mali,34 providing more than 18 million USD in immunization programming support in 2018, including health systems strengthening funds and new and under-used vaccine support for the pentavalent vaccine, pneumococcal conjugate vaccine, inactivated polio vaccine (IPV), rotavirus vaccine, and yellow fever vaccine (Figure 12).
Source: Gavi, the Vaccine Alliance Disbursement Data, 2022.
In addition to Gavi, important development partners for immunization in Mali include UNICEF, the Canadian International Development Agency (CIDA), WHO, and the United States Agency for International Development (USAID).35,36
Mali’s routine immunization strategies are established primarily by the Ministry of Health and Public Hygiene (MSHP). The MSHP develops national health policies, including those related to routine immunization, and is responsible for overseeing health systems and setting norms and standards. The National Health Directorate (DNS) is situated under the MSHP and plays a role in allocating immunization resources and implementing the policies established by the MSHP. Routine immunization activities such as immunization campaigns are the responsibility of the National Immunization Center and Regional Health Directorates with the support of national associations and external partner organizations.
Mali’s Center for Vaccine Development (CVD) falls under the MSHP and is responsible for testing the safety and efficacy of new vaccines, distributing vaccines, training vaccinologists, and quantifying disease burden for decision makers. The CVD partners with international organizations and NGO stakeholders. Other government agencies such as the National Center for Information, Education, and Communication (CNIECS) are responsible for coordinating and implementing immunization promotion strategies and plans.
National Policies
Mali’s latest Plan Décennal de Développement Sanitaire et Social (PDDSS) is the government’s main document for outlining immunization-related priorities. The latest PDDSS was developed for the period 2014-2023 and describes priorities and strategies for Mali’s immunization programming.
The 2014-2023 PDDSS describes achievements that were made following the implementation of the previous PDDSS (1998-2007), including a reduction in infant mortality, an increased number of community-level vaccine delivery sites, and the introduction of free pre- and post-natal care.
The PDDSS also describes immunization-related gaps that remained following implementation, including poor geographic coverage of community-level vaccine delivery sites, frequent vaccine stock outs and inadequate vaccine storage at the community level, inadequate staffing at vaccine delivery sites, and inequities in vaccination coverage. National objectives set forth in the plan include reducing morbidity and mortality from communicable diseases, reducing vaccine stockouts, increasing Penta3 coverage to 98 percent, increasing the percentage of health funding allocated to the poorest areas to 60 percent, eliminating measles, polio, and meningitis, and strengthening epidemiological surveillance. The PDDSS does not describe any strategies specifically targeting ZD children. However, strategies to achieve the broader immunization objectives include strengthening community-level health services by employing more community health agents who can respond to the social and cultural contexts of their service areas; establishing national quality standards for care at the health facility level; strengthening vaccine storage and management capacity at community-level sites; and introducing a national import mechanism for vaccines.
The PDDSS places a strong focus on strengthening community-level health systems as a strategy for reaching rural, sparsely populated and/or hard-to-reach areas, and nomadic communities for immunization. Table 3 summarizes key government documents that address immunization and outline specific activities and targets.
Table 3. National Policy and Strategy Documents Relevant to Immunization
| Policy/Legislation | Year/s | Summary |
|---|---|---|
| Plan Décennal de Développement Sanitaire et Social (PDDSS) | 2014-2023 | The government’s 10-year plan for Mali’s health and social development sectors. The plan establishes immunization objectives and strategies, including increasing Penta3 coverage to 98 percent and eliminating measles, polio, and meningitis. The plan also outlines strategies for strengthening health systems at the community level and improving vaccine management. It is the strategic framework for the Programme de Développement Socio-Sanitaire (PRODESS III). |
| Programme de Développement Socio-Sanitaire (PRODESS IV) | 2020-2023 | The PRODESS IV is the program through which the second five-year phase of the PDDSS 2014-2023 is implemented. The program includes strategic outcomes for implementing the PDDSS’ objectives and outlines progress following PRODESS II. |
| Programme de Développement Socio-Sanitaire (PRODESS III) | 2014-2018 | The PRODESS III is the program through which the first five-year phase of the PDDSS 2014-2023 was implemented. The program includes 62 strategic outcomes for implementing the PDDSS’ objectives including the introduction of new vaccines. |
| Loi d'orientation sur la santé (Health Orientation Law) | 2018 | This law, established by the Government of Mali, establishes broad guidelines for national health policy. Its primary objectives are to improve the performance of the health system, extend health coverage, and improve the health of Malians. The law was first established in 2002 and undergoes periodic updates, with the most recent update taking place in 2018. |
| Politique Nationale de Développement des Ressources Humaines pour la Santé | 2009-2015 | This policy was created by the Ministry of Health in response to a shortage of human resources for health in the Malian health system. It lays out strategies for training, recruiting, and motivating health staff, including those at community-level immunization sites. |
| Plan Décennal de Développement Sanitaire et Social (PDDSS)+ PRODESS I & PRODESS II | 1998-2007 | The PDDSS is Mali’s 10-year plan for the health and social development sectors. It was implemented through two five-year programs (the PRODESS I and PRODESS II). The plan and its implementation programs outline methods for decentralizing the health system. |
Human Resources for Health
Adequate human resources are essential for all health care services, including immunization services. However, immunization programs require a range of staff, including clinicians, supply chain professionals, logisticians, cold chain technicians, and data entry staff. In Mali, community health agents are the primary providers of immunization services37 and are assisted by community health center staff and community health association members. As of 2016, one community health agent was available for every 700 people in Southern Mali and every 100-500 people in Northern Mali.38 Despite having a higher ratio of health agents to patients, geographic accessibility remains a challenge in rural and hard-to-reach areas of Northern Mali.39 The national 10-year plan details initiatives to increase geographic accessibility to community health agents as well as initiatives to strengthen health service provider training and health workforce data for improved decision-making. Data from the WHO National Health Workforce Accounts database indicate that the ratio of community health workers increased from 0.08 per 10,000 people in 2009 to 1.56 per 10,000 people in 2020, in part due to Mali’s 2009 National Human Resources Development Policy for Health (Politique Nationale de Développement des Ressources Humaines pour la Santé en 2009) which called for recruitment of community health personnel. The ratio of midwifery and nursing personnel, however, decreased between 2009 and 2020.40
Analyses of the adequacy of staffing of non-clinical professionals like community health agents are largely absent from the literature. This may be an area of further investigation by the CLHs.
Health Management Information System Structure and Disaggregation, Data Availability, and Use
Mali’s District Health Information Software 2 (DHIS2) system was established in 2016 and by 2019, the system had been deployed in 100 percent of Mali’s regions, hospitals, and health districts, and 98 percent of community health centers.41 In 2013, prior to DHIS2 deployment, an assessment of Mali’s health management information systems (HMIS) found that the overall quality of the country’s health data was poor, particularly at the lower levels of the health system. Issues with data accuracy and completeness were due in part to poor data archiving and record keeping.42 Additionally, each sector of the health system managed its own HMIS, creating a fragmented data management system that led to a heavy data collection burden for healthcare service providers. Deployment of DHIS2 led to the integration of all health information subsystems, including those previously managing immunization data. Between 2016 and 2019, national estimates of data completeness increased from 74.5 percent to 97 percent and timeliness increased from 5.7 percent to 70.9 percent.43 There is likely variation in data quality at subnational levels that is not captured in the literature. In 2022, Mali began a process of integrating its electronic Logistics Management Information Systems (eLMIS) with its national DHIS2 system to improve supply chain management and allow both vaccination data and supply data to be collected at the facility level. As of February 2023, 67 percent of health districts in Mali are utilizing the new integrated system.44
Immunization data in Mali is collected at community-level health facilities or the sites of community-level immunization campaigns, which are overseen by Community Health Associations (Association de Santé Communautaire—ASACOs). Community health workers collect paper-based data, which are then submitted to the district level, aggregated and reviewed, and then sent to the regional level and finally to the national level.45 Electronic vaccination registries were piloted at two community health facilities in 2017 and have since been extended to all facilities in two districts, with the intention of further scale up.46
A number of initiatives to improve the quality of HMIS data have been introduced in Mali, including technical training on DHIS2 for staff at all levels of the health system, the introduction of electronic registration tools, and data validation activities.47 Despite these initiatives, limited telecommunications connectivity across the country, particularly in northern and rural areas, hinders both electronic data collection and the ability to provide comprehensive training. As of 2020, just 16 percent of the rural population in Mali had access to electricity compared to 94 percent of urban population.48
Comprehensive data quality assessments of immunization data in Mali post-DHIS2 deployment were not identified in the literature. This may be an area for further study.
Community health structure and role in routine immunization
Mali’s community health structure is guided in part by the country’s National Implementation Guide for Essential Community Health Care (Soins essentiels dans la communauté: Guide national pour la mise en oeuvre [SEC]). Developed in 2015, the SEC outlines the roles and responsibilities of community health providers and the processes for delivering and managing immunization services.There are two main cadres of community health providers in Mali: agents de santé communautaire (ASC) and relais communautaires (relais). Both cadres are linked to a community health center, or Centre de Santé Communautaire (CSCOM), and are supervised by a Health Center Technical Director. ASCs are paid workers recruited by a CSCOM committee and are responsible for delivering vaccination and other basic maternal, newborn, and child health (MNCH) and water, sanitation, and hygiene (WASH) interventions. Relais are unpaid volunteers selected by the communities in which they live whose primary role is to assist the ASC in service delivery, community mobilization, and health promotion. Formal systems for the training and support of relais do not exist, though in some cases, they may receive stipends from non-governmental sources.
Immunization Program Details
The Expanded Programme for Immunization (EPI) in Mali is implemented primarily through Centres de Santé Communautaire (CSCOMs), outreach events at community sites, and vaccination campaigns. As shown in Figure 13, Each CSCOM is non-profit and is created and managed by an ASACO at the community level. Mali’s two main cadres of community health providers, community health agents (l’agent de santé communautaire – ASC) and relais, are assigned to service areas for which they provide immunization services. With the support of ASACOs, ASC and relais mobilize communities for vaccination, conduct vaccination outreach, and provide vaccination reminders. The primary service delivery site varies between each service area depending on the geographic accessibility of the CSCOM. In many cases, particularly in rural areas, vaccines are delivered at fixed community sites or in mobile medical units.
Figure 13. Organization of Mali’s Health System
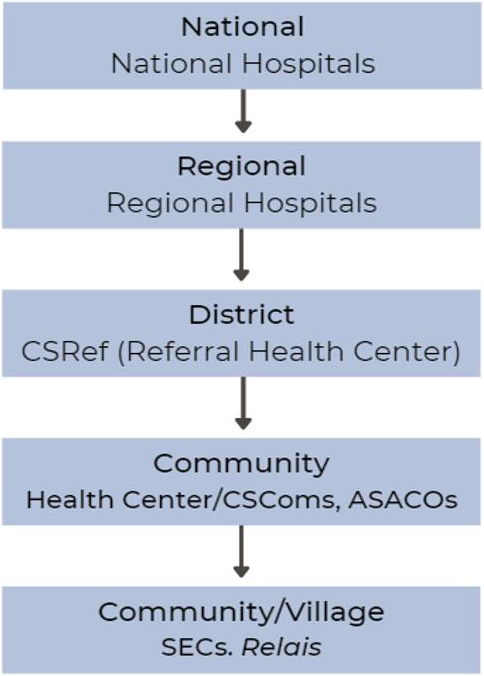
The EPI in Mali was established in 1986 and its activities are funded by the public and private sectors, including the government, the Ministry of Health, technical and financial partners, and NGOs. CSCOMs are managed, financed, and operated by the communities they serve, with many receiving assistance from partners.
Environmental Context
Impact of Northern Conflict on Routine Health Services
In early 2012, longstanding tensions between the Mouvement National pour la Libération de l’Azawad (MNLA) and the government in northern Mali were exacerbated by the sudden arrival of Libyan armed fighters to the region following the collapse of Libya. The MNLA, along with other groups based in West Africa and Algeria, sought to garner public support against the Malian government and create an independent state in northern Mali. Following a coup d’état, the MNLA proclaimed northern Mali’s independence. Shortly after, additional violent conflicts emerged between the MNLA and competing political and ethnic factions. Despite a peace agreement signed in 2015, the region remains unstable due to fighting between armed groups and the national army.49
Health service delivery was severely disrupted in the region at the onset of the conflict, including routine immunization service delivery.50 The ongoing violence and instability in the region continue to pose challenges to service delivery in northern Mali. As of 2019, an estimated 17 percent of health structures in conflict-affected regions were no longer functioning.51 However, the logistics of reaching conflict zones makes it challenging to assess the extent to which health services in the region continue to be disrupted. Despite evidence that community health workers are successful in reaching remote communities in zones controlled by armed groups, the support is challenging to monitor.52 Additionally, an estimated 200,000 people in Mali have been internally displaced as a result of the conflict.53 Studies investigating the impact of health service disruptions on those displaced are limited.
Many international development operations in the region became decentralized as a result of the conflict. The difficulties accessing conflict zones and the complex relationships between the government and competing factions in northern Mali shifted many health program operations to local NGOs.54 A lack of coordination between the decentralized and fragmented health programs across the region may have had an impact on immunization coverage in the region.55
Immunization Partners and Zero Dose Efforts
Table 4 below shows a list of immunization stakeholders engaged in ZD efforts in Mali. The content will be expanded in future iterations of the landscape through a series of planned KIIs with stakeholders at national and subnational levels.
Table 4. List of Preliminary Stakeholders in Immunization
| Sl. No. | Organization/Entity | Category | Geographic coverage | Dates of work | Funder | Description of work |
|---|---|---|---|---|---|---|
| 1 | United Nations International Children's Emergency Fund (UNICEF)- Mali | Funder/ Technical Assistance | International | 1960-present | UNICEF | To support the country’s efforts to respond to the most vulnerable children, including working with all levels of government to provide immunization services. |
| 2 | World Health Organization (WHO) | Funder/ Technical Assistance | International | 1960-present | WHO | To provide technical advice and support to improve the health and development of Malians, including monitoring and assessing trends in health indicators. |
| 3 | United States Agency for International Development (USAID) | Funder | International | 1961-present | U.S. government | To strengthen Mali’s capacity to deliver Maternal, Newborn, and Child Health (MNCH) services, including immunization delivery. |
| 4 | World Bank | Funder | International | 1963-present | The International Development Association (IDA) | To support Mali’s development including poverty reduction and economic recovery. |
| 5 | World Vision International | Technical Assistance | International | 1975-present | A combination of support from private funders and multilateral agencies, including UNICEF, WHO, and World Bank, among others. | To promote childhood immunization at the community-level through behavior change communications. |
| 6 | National Institute of Public Health (INSP) (formerly INRSP) | Government | National | 1981-present | Ministry of Health and Hygiene | To establish Mali’s systems for health monitoring and epidemiological surveillance. |
| 7 | National Immunization Center | Government | National | 1990-present | Ministry of Health and Hygiene | To evaluate Mali’s EPI and develop standards and procedures for disease control. |
| 8 | Center for Study and Research on Child Survival (CREDOS) | Research and Implementation | National | 2000-present | Ministry of Health and Hygiene | National research body committed to promoting research related to child survival and well-being. |
| 9 | Gavi | Funder | International | 2001-present | Gavi | To fund initiatives to promote vaccination of children against deadly and debilitating infectious diseases. |
| 10 | Center for Vaccine Development in Mali (CVD-Mali) | Research and Implementation | National | 2001-present | Bill & Melinda Gates Foundation (BMGF), CDC Foundation, The European & Developing Countries Clinical Trials Partnership (EDCTP), WHO, among others | To support Mali’s efforts to improve the health of its communities through research, vaccine development and distribution, and surveillance. |
| 11 | National Institute for Statistics (INSTAT) | Government | National | 2009-present | Ministry of Health and Hygiene | Collects, analyzes, and disseminates Malian health-related data. |
| 12 | Dalberg | Technical Assistance | International | 2014-present | To strengthen Mali’s disease surveillance and response systems. | |
| 13 | PATH | Technical Assistance | International | 2016-present | U.S. government, UNICEF, Gavi, WHO, among others | Supports the development, delivery, and introduction of vaccines. Includes a focus on ZD children. |
| 14 | Clinton Health Access Initiative (CHAI) | Research and Implementation | International | 2019-present | Gavi | CHAI works with the Mali Ministry of Health and Public Hygiene to increase access to quality healthcare at CSComs. |
| 15 | MOMENTUM Integrated Health Resilience | Technical Assistance | International | 2020-present | USAID | To increase the availability and utilization of essential health services, including immunization, with a focus on northern regions of the country. |
| 16 | GaneshAID | Technical Assistance | International | 2022-present | Gavi | Supports the creation of a community of practice focused on improving immunization systems. |
| 17 | Health Information Service Provider (HISP) West and Central Africa in Mali | Technical Assistance | International | 2022-present | USAID | Supports DHIS2 implementation and capacity building in Mali. |
| 18 | Zero-Dose Immunization Programme | Technical Assistance | International | 2022-present | Gavi | To identify and vaccine ZD children in conflict settings through the Reaching and Adapting Immunization Services Effectively to reach Zero-Dose Children in the Sahel (RAISE 4 Sahel) project. |
Relevant Resources
Below are several relevant resources related to health and immunization in Mali, including surveys, data, reports, and databases.
Surveys
Immunization and Health Data
Program Reports, National Strategies and Databases
- Mali Plan Décennal de Développement Sanitaire et Social (PDSS) 2014-2023
- Plan Strategy National de communication du Programme Elargi de Vaccination (PEV) 2017-2020
- Global Health Expenditure Database - 2022 Release
- HeRAMs report 2020, 2022
- Urban Strategy 2019
- SARA Report 2018
- Dossier D’investissement Pour L’acceleration de la Vaccination Plus au Mali | UNICEF
Anticipated Work/Publications
- Mali Demographic and Health Survey 2023-24
References
1 The DHS Program STATcompiler. Funded by USAID. (Accessed April 3 2023).
2 Institute for Health Metrics and Evaluation (IHME). GBD Results, Mali. Seattle, WA: IHME, University of Washington, 2020. (Accessed April 3 2023).
3 The DHS Program STATcompiler. Funded by USAID. (Accessed April 3 2023).
4 Dimitrova, A., Carrasco-Escobar, G., Richardson, R., Benmarhnia, T. (2023) Essential Childhood Immunization in 43 Low- and Middle-income Countries: Analysis of Spatial Trends and Socioeconomic Inequalities in Vaccine Coverage. PLoS Med20(1): e1004166.
5 United Nations, Department of Economic and Social Affairs, Population Division. 2022. “World Population Prospects 2022, Online Edition.”
6 United Nations Inter-agency Group for Child Mortality Estimation (2023).
7 Li, X., Mukandavire, C., Cucunubá, Z. M., Londono, S. E., Abbas, K., Clapham, H. E., Jit, M., Johnson, H. L., Papadopoulos, T., Vynnycky, E., Brisson, M., Carter, E. D., Clark, A., Villiers, M. J. de, Eilertson, K., Ferrari, M. J., Gamkrelidze, I., Gaythorpe, K. A. M., Grassly, N. C., … Garske, T. (2021). Estimating the Health Impact of Vaccination Against Ten Pathogens in 98 Low-Income and Middle-Income Countries from 2000 to 2030: A Modelling Study. The Lancet, 397(10272), 398–408.
9 Tapia, M.D., Sylla, M., Driscoll, A.J., Touré, A., Kourouma, N., Sissoko, S., Tamboura, B., Diakité, A.A., Panchalingam, S., Keïta, A.M., Tennant, S., Onwuchekwa, U., Roose, A., Deloria Knoll, M., Higdon, M.M., Prosperi, C., Hammitt, L.L., Feikin, D.R., Murdoch, D.R., O'Brien, K.L., Sow, S.O., Kotloff, K.L. The Etiology of Childhood Pneumonia in Mali: Findings From the Pneumonia Etiology Research for Child Health (PERCH) Study. Pediatr Infect Dis J. 2021 Sep 1;40(9S):S18-S28. doi: 10.1097/INF.0000000000002767. PMID: 34448741; PMCID: PMC8448406.
10 Gavi Secretariat. 2023. “Mali Zero Dose Analysis.” Unpublished.
11 Ibid.
12 Ibid.
13 Ibid.
14 Ibid.
15 Bonnet, E., Bodson, O., Le Marcis, F., Faye, A., Sambieni, N. E., Fournet, F., Boyer, F., Coulibaly, A., Kadio, K., Diongue, F. B., & Ridde, V. (2021). The COVID-19 Pandemic in Francophone West Africa: From the First Cases to Responses in Seven Countries. BMC Public Health, 21, 1490.
16 Amouzou, A., Maïga, A., Faye, C. M., Chakwera, S., Melesse, D. Y., Mutua, M. K., Thiam, S., Abdoulaye, I. B., Afagbedzi, S. K., Iknane, A. A., Ake-Tano, O. S., Akinyemi, J. O., Alegana, V., Alhassan, Y., Sam, A. E., Atweam, D. K., Bajaria, S., Bawo, L., Berthé, M., … Boerma, T. (2022). Health service Utilisation During the COVID-19 Pandemic in Sub-Saharan Africa in 2020: A Multicountry empirical Assessment with a Focus on Maternal, Newborn and Child Health Services. BMJ Global Health, 7(5), e008069.
17 Shapira, G., Ahmed, T., Drouard, S. H. P., Amor Fernandez, P., Kandpal, E., Nzelu, C., Wesseh, C. S., Mohamud, N. A., Smart, F., Mwansambo, C., Baye, M. L., Diabate, M., Yuma, S., Ogunlayi, M., Rusatira, R. J. D. D., Hashemi, T., Vergeer, P., & Friedman, J. (2021). Disruptions in Maternal and Child Health Service Utilization During COVID-19: Analysis from Eight Sub-Saharan African Countries. Health Policy and Planning, 36(7), 1140–1151.
18 Amouzou, A., Maïga, A., Faye, C. M., Chakwera, S., Melesse, D. Y., Mutua, M. K., Thiam, S., Abdoulaye, I. B., Afagbedzi, S. K., Iknane, A. A., Ake-Tano, O. S., Akinyemi, J. O., Alegana, V., Alhassan, Y., Sam, A. E., Atweam, D. K., Bajaria, S., Bawo, L., Berthé, M., … Boerma, T. (2022). Health Service Utilisation During the COVID-19 Pandemic in Sub-Saharan Africa in 2020: A Multicountry Empirical Assessment with a Focus on Maternal, Newborn and Child Health Services. BMJ Global Health, 7(5), e008069.
19 World Bank. 2021. Mali Economic Update, Spring 2021: Protecting the Vulnerable During the Recovery. World Bank, Washington, DC.
20 Amouzou, A., Maïga, A., Faye, C. M., Chakwera, S., Melesse, D. Y., Mutua, M. K., Thiam, S., Abdoulaye, I. B., Afagbedzi, S. K., Iknane, A. A., Ake-Tano, O. S., Akinyemi, J. O., Alegana, V., Alhassan, Y., Sam, A. E., Atweam, D. K., Bajaria, S., Bawo, L., Berthé, M., … Boerma, T. (2022). Health Service Utilisation During the COVID-19 Pandemic in Sub-Saharan Africa in 2020: A Multicountry Empirical Assessment with a Focus on Maternal, Newborn and Child Health Services. BMJ Global Health, 7(5), e008069.
21 World Bank. 2021. Mali Economic Update, Spring 2021: Protecting the Vulnerable During the Recovery. World Bank, Washington, DC.
22 Assaf, Shireen, Lwendo Davis Moonzwe, Ahamadou Diallo, and Amadou Kone. 2020. Trends in and Factors Associated with Maternal and Child Health Indicators in Mali: Further Analysis of the Mali Demographic and Health Surveys 2006-2018. DHS Further Analysis Reports No. 131. Rockville, Maryland, USA: ICF.
23 United Nations Children’s Fund, The State of the World’s Children 2023: For Every Child, Vaccination, UNICEF Innocenti – Global Office of Research and Foresight, Florence, April 2023.
24 Mali Demographic and Health Survey 2018. Bamako, Mali, and Rockville, Maryland, USA: INSTAT and ICF.
25 Ataullahjan, A., Gaffey, M.F., Sami, S., Singh, N.S., Tappis, H., Black, R.E., Blanchet, K., Boerma, T., Langer, A., Spiegel, P.B., Waldman, R.J., Wise, P.H., Bhutta, Z.A.. C’est Vraiment Compliqué: a Case Study on the Delivery of Maternal and Child Health and Nutrition Interventions in the Conflict Affected Regions of Mali. Conflict and Health. 2020;14(1).
26 Degni, F., Amara, I.D., Klemetti, R.. Women’s Experiences in Accessing Maternal and Child Health Services During the Period of the Armed Conflict in the North of Mali. Open Public Health J. 2015;8:1.
27 Devlin, K., Farnham Egan, K., & Pandit-Rajani, T., “Community Health Systems Catalog Country Profile: Mali.,” Advancing Partners & Communities., Arlington, VA, 2016.
28 WHO Global Health Expenditure Database. Health Expenditure Profile, Mali.
29 Arsenault, C., Johri, M., Nandi, A., Mendoza Rodríguez, J.M., Hansen P.M., Sam Harper, S. 2017. “Country-Level Predictors of Vaccination Coverage and Inequalities in Gavi-Supported Countries.” Vaccine 35 (18): 2479 88.
30 Wagstaff, A., Eozenou, P., & Smitz, M.. 2019. “Out-of-Pocket Expenditures on Health,” April.
31 Sim, S.Y., Watts, E., Constenla, D., Brenzel, L., & N. Patenaude, B.N. 2020. “Return On Investment From Immunization Against 10 Pathogens In 94 Low- And Middle-Income Countries, 2011–30.” Health Affairs 39 (8): 1343–53.
32 WHO Immunization Data Portal.
33 Gavi the Vaccine Alliance. 2023. “Eligibility.”
34 Dossier D’Investissement Pour L’Acceleration De La Vaccination Plus Au Mali | UNICEF. (2019, January 1).
35 Ibid.
36 Mounier-Jack, S., Burchett, H. E. D., Griffiths, U. K., Konate, M., & Diarra, K. S. (2014). Meningococcal Vaccine Introduction in Mali Through Mass Campaigns and its Impact on the Health System. Global Health, Science and Practice, 2(1), 117–129.
37 Devlin, K., Farnham Egan, K., & Pandit-Rajani, T. “Community Health Systems Catalog Country Profile: Mali.,” Advancing Partners & Communities., Arlington, VA, 2016.
38 Ibid.
39 Plan Décennal de Développement Sanitaire et Social (PDDSS) 2014-2023. Ministère de la Santé et de l’Hygiène Publique.
40 The National Health Workforce Accounts database, World Health Organization, Geneva.
41 MEASURE Evaluation. (2019). L’expérience du Mali dans le déploiement du DHIS2.
42 MEASURE Evaluation. Evaluation du Système Local d’Information Sanitaire (SLIS) avec les Outils PRISM: Rapport. MEASURE Evaluation; 2014. (Accessed May 6, 2023).
43 Ibid.
44 Chikwado. (2023, April 3). Mali Implements an Integrated eLMIS Leveraging DHIS2 and MEDEXIS for Real-time Logistics Management. DHIS2.
45 Devlin, K., Farnham Egan, K., & Pandit-Rajani, T. “Community Health Systems Catalog Country Profile: Mali.,” Advancing Partners & Communities., Arlington, VA, 2016.
46 Strengthening Health Information Systems in Mali—MEASURE Evaluation. (2019). [Publication]. Retrieved May 3, 2023.
47 MEASURE Evaluation. (2019). L’expérience du Mali dans le déploiement du DHIS2.
48 The World Bank website. World Development Indicators page, 2020.
49 Ataullahjan, A., Gaffey, M. F., Tounkara, M., Diarra, S., Doumbia, S., Bhutta, Z. A., & Bassani, D. G. (2020). C’est Vraiment Compliqué: A Case Study on the Delivery of Maternal and Child Health and Nutrition Interventions in the Conflict-Affected Regions of Mali. Conflict and Health, 14(1), 36.
50 Masset, E. (2022). Conflict and Child Mortality in Mali: A Synthetic Control Analysis. Population and Development Review, 48(4), 1097–1123.
51 Providing Healthcare in Armed Conflict: The Case of Mali | International Peace Institute. (2019). Retrieved June 19, 2023.
52 Ibid.
53 OCHA. Mali—3,5 Millions de Personnes sont Actuellement en Insécurité Alimentaire ou à RIsque D’insécurité Alimentaire | Digital Situation Reports. (2019). Retrieved June 19, 2023.
54 Ataullahjan, A., Gaffey, M. F., Tounkara, M., Diarra, S., Doumbia, S., Bhutta, Z. A., & Bassani, D. G. (2020). C’est vraiment compliqué: A Case Study on the Delivery of Maternal and Child Health and Nutrition Interventions in the Conflict-Affected Regions of Mali. Conflict and Health, 14(1), 36.
55 Masset, E. (2022). Conflict and Child Mortality in Mali: A Synthetic Control Analysis. Population and Development Review, 48(4), 1097.