Nigeria Zero-Dose Landscape

Background
The Gavi Zero-Dose Learning Hub (ZDLH) is responsible for highlighting the work produced by the four Gavi, the Vaccine Alliance Country Learning Hubs (CLHs) in Bangladesh, Mali, Nigeria, and Uganda with the objective of using this evidence to better understand the factors influencing implementation and performance of approaches to identify and reach zero-dose (ZD) and under-immunized (UI) children as well as missed communities. The consortium, led by JSI in partnership with the International Institute of Health Management Research (IIHMR) and The Geneva Learning Foundation (TGLF), aims to support CLHs to implement Gavi’s identification, reach, monitoring, measurement, and advocacy (IRMMA) Framework; facilitate sharing and learning across the CLHs; contribute evidence to capture, synthesize, and disseminate the breadth of learning across the Vaccine Alliance; and, ultimately, help improve immunization equity and reduce the number of ZD and UI children globally through quality evidence generation and uptake.
In pursuit of these objectives, the ZDLH has developed ZD landscapes to synthesize the evidence to date on immunization prevalence, policy, and programming in each of the four CLH countries. The landscapes describe the current immunization and ZD context, including coverage trends, equity, health systems, and existing partners and programming, to orient implementers and funders to the broad immunization context and opportunity for intervention to reduce the prevalence of ZD children. While this landscape presents the findings of syntheses of existing literature, the CLHs in Nigeria and other countries will generate evidence based on their own country-level ZD programming and activities including rapid assessments and surveys.
The purpose of this landscape is to provide the Gavi CLH and stakeholders in Nigeria with a comprehensive overview of the immunization landscape within the country, with a special focus on ZD and UI children. Gavi defines a ZD child as one who has not received a single dose of a diphtheria, tetanus, and pertussis-containing vaccine. Given the highly variable and contextual nature of the drivers, barriers, and programmatic approaches to reach ZD and UI children, it is important to understand the unique context, policies, and economics of the country to help guide approaches, as well as to better understand and interpret why changes in IRMMA may or may not occur. This landscape also aims to inform research and programming efforts in Nigeria by identifying important knowledge gaps that pertain to the identification, reach, monitoring, measurement, and advocacy for ZD and UI children.
Methods
The ZD landscape assessments are based on literature reviews and secondary data analyses. The ZDLH team identified relevant literature by searching both gray and peer-reviewed sources, ministry and partner websites, and existing Gavi reviews and resources. Domains of interest included immunization coverage, equity, and information about the health system in which the immunization program operates including, but not limited to, human resources, financing, immunization policies, and the overall health system structure. The team identified and reviewed relevant publications identified and reviewed and extracted information related to the ZD or immunization context in each country. Where gaps in information remain, the team relied on input from CLHs and key informant interviews (KIIs) conducted as part of the complementary political economy analysis (PEA). These landscapes are intended to represent the current situation in the countries and will be updated on an annual basis with new resources including those generated by the CLHs.
Introduction
Nigeria has made progress in improving vaccination coverage over the last two decades, with the percentage of children aged 12–23 months who have received their basic vaccination increasing from 23 percent in 2008 to 44 percent in 2021.1,2 Additionally, the country achieved an important milestone in 2020 when it was designated polio-free. However, Nigeria needs to make significant progress to reach its national target of achieving an average national coverage of 80 percent by 2028.3,4 According to 2022 estimates from the United Nations Children’s Fund (UNICEF) and the World Health Organization (WHO), Nigeria has 2.3 million children who have not been immunized (also known as ZD children), the second highest number in the world.5 Immunization coverage varies widely across Nigeria and is lowest in the North, an area of the country that has been particularly affected by armed conflict and displacement.6,7 Identifying approaches to tracking and reaching these children is critical to reaching full and equitable immunization coverage in Nigeria.
Nigeria is located in West Africa, bordered by Niger, Chad, Cameroon, and Benin (Figure 1). It is Africa’s most populous country, with a population of almost 219 million people in 2022, of which approximately 35 million are children under five (Table 1).8
Figure 1. Map of Nigeria

Table 1. Total Population and Residence
| Total Population (2021) | |
|---|---|
| Total | 218,541,212 |
| Male | 110,448,137 |
| Female | 108,093,075 |
| Residence (2021) | |
|---|---|
| Rural | 46% |
| Urban | 54% |
Source: World Bank Open Data. “World Bank Open Data.” Accessed August 2, 2023.
Despite progress toward reducing mortality in children under five in Nigeria (Figure 2), Nigeria had the highest number of deaths of children under five in the world in 2020.9 The United Nations Inter-agency Group for Child Mortality Estimation estimates that more than 852,000 children died in 2021, many from preventable causes including vaccine-preventable diseases.10
Source: United Nations Inter-agency Group for Child Mortality Estimation (2023).
The 2019 Global Burden of Disease study found that at least 41 percent of deaths among children under five in Nigeria may be vaccine-preventable, including diarrheal diseases, lower respiratory infections, and meningitis (Figure 3).11
Source: Institute for Health Metrics and Evaluation (IHME). GBD Results, Nigeria. Seattle, WA: IHME, University of Washington, 2020. (Accessed July 2023).
Improved access to immunization is a principal driver of the decrease in under-five mortality in developing countries. Three decades of routine immunization programs have contributed to dramatic declines in vaccine-preventable diseases such as measles in countries like Nigeria (Figure 4).
Source: IHME. GBD Results, Nigeria. Seattle, WA: IHME, University of Washington, 2020. (Accessed July 2023); World Health Organization. Global Health Observatory data repository: Measles containing vaccine first-dose (MCV1) immunization coverage among 1-year-olds. 2023. (Accessed July 2023).
Immunization Context
Despite increases in vaccination coverage over time, gaps in immunization continue to contribute to under-five morbidity and mortality in Nigeria. Gavi estimates children who have not received a single dose of the pentavalent (Penta) vaccine series represent 39 percent of all deaths (336,925 total deaths) among children under five in the country.12
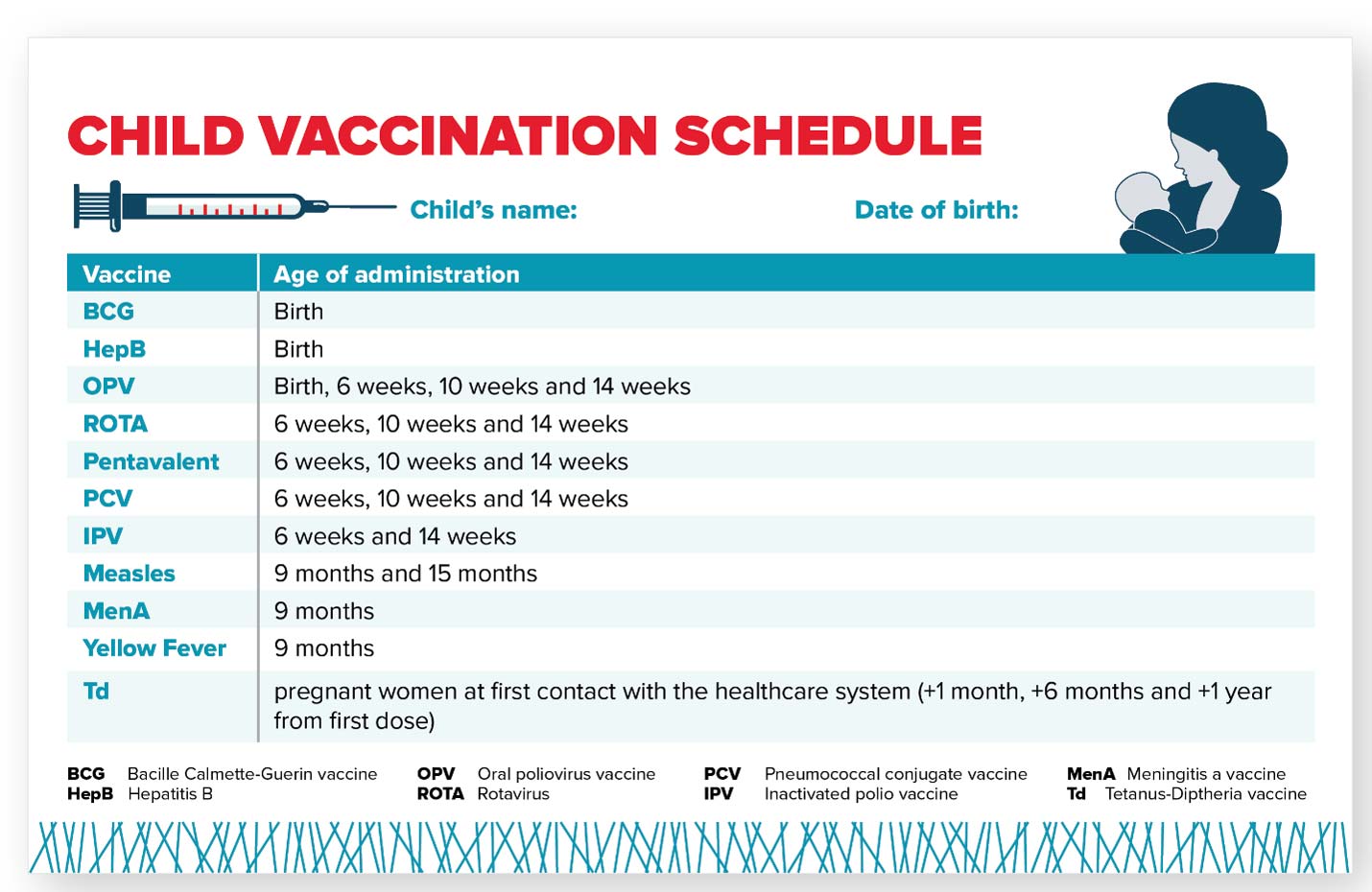
Immunization Schedule
Nigeria’s immunization schedule includes 11 different vaccines and targets approximately eight million children each year (Figure 5). Operationally, Gavi defines a ZD child as one who has not received a single dose of a diphtheria, tetanus, and pertussis-containing vaccine. Nigeria administers the Penta vaccine, which protects against diphtheria, tetanus, pertussis, hepatitis B, and Haemophilus influenzae type b (Hib). In Nigeria and for the purposes of this landscape, ZD children are defined as those who have not received a single dose of the Penta vaccine series.
Figure 5. Nigeria Childhood Vaccination Schedule
Coverage Estimates
Current coverage estimates for six basic immunizations in Nigeria are presented in Figure 6. Coverage ranges from 75 percent of children receiving BCG at birth to only 36 percent of children receiving the second dose of a measles containing vaccine (MCV) at 15 months of age. Identifying and reaching ZD and UI children in Nigeria is essential to meet the Gavi 5.0 equity goal and progress toward reaching all eligible children with routine vaccination in the country.
Source: World Health Organization/UNICEF Estimates of National Immunization Coverage (WUENIC)—2022 estimates. (2023). WHO Immunization Data Portal.
Estimating the number of ZD children in Nigeria requires estimates of Penta1 coverage and the total number of surviving children. These can vary based on the source of the data, resulting in different estimates of the ZD population (Table 2). Positive estimates (those above zero) range from 1.21 million (from Nigeria’s national administrative data) to 2.25 million ZD children (from WHO/UNICEF Estimates of National Immunization Coverage [WUENIC]).12
Table 2. Nigeria ZD Estimate Inputs
| Source | Total Number of Surviving Infants | Penta1 Coverage | Number of ZD Children |
|---|---|---|---|
| WUENIC (2022) | 7,570,882 | 70% | 2,271,265 |
| IHME (2021) | 7,490,708 | 74% | 1,947,584 |
| Administrative data (2021) | 8,036,751 | 85% | 1,205,513 |
Source: Gavi MEL Team. (2023). Nigeria Zero Dose Analysis; World Health Organization/UNICEF Estimates of National Immunization Coverage (WUENIC)—20221 estimates. (2023). WHO Immunization Data Portal.
While Nigeria’s administrative data from 2021 provides a positive estimate of ZD children nationally, this is not the case at the subnational level, where 206 districts (out of 774) have coverage rates of over 100 percent, resulting in a negative number of ZD children.12 Coverage rates of over 100 percent could indicate data quality issues or inaccurate population data. The Federal Government of Nigeria has recognized the challenges associated with using administrative data and, for the first time, has decided to use survey data rather than administrative data for estimates and programming.3
The goal of WUENIC analyses is to provide national immunization estimates on an annual basis. WUENIC immunization estimates are developed by triangulating data from several sources including government data, published and unpublished survey data, and consultation with local experts and governments. Statistical and mathematical modeling are not used to derive the final coverage estimates and estimates are not available at the sub-national level.13 As such, WUENIC estimates are not useful for identifying the location of ZD children in the country, but rather for looking at trends in the ZD population over time.
Institute for Health Metrics and Evaluation (IHME) projections include different inputs and analyses because IHME generates highly-specific geospatial estimates of immunization coverage that are combined with additional data to generate national coverage estimates. IHME, like WUENIC, uses household survey data as well as national data, but it also uses covariates of immunization (such as residence or mother’s level of education) when calculating estimates. Using this data, IHME models immunization coverage at a hyper-local level (a five-by-five kilometer [km] area) and then incorporates additional higher-level data to model a national estimate.12 The resulting estimates provide more insight into the probable locations of ZD children within a country, but also include more assumptions and potential errors than estimates generated from household surveys or administrative data. Given the differences in source data and estimation approaches, the true number (and location) of ZD children is not known. However, by triangulating the various estimates, we can determine where there is overlap and generate an informed best guess to use for broad planning purposes. Tailored implementation strategies to vaccinate ZD children may require other methods to better understand where they are located, how to reach them, and how to effectively bring them into routine immunization services.
For the purposes of this landscape, we will use data from both WUENIC and IHME sources with the understanding that the estimates are imperfect. Data from household surveys, like the Nigeria Demographic and Health Surveys (DHS) and the Multiple Indicator Cluster Survey (MICS), will also be incorporated into this assessment, particularly for equity analyses.
Effects of the COVID-19 Pandemic
Nigeria implemented several COVID-19 mitigation and containment strategies following its first case on February 27, 2020, including travel restrictions, bans on large gatherings, and closures of schools, markets, and places of worship. Globally, as well as in Nigeria, these strategies have been shown to have a deleterious effect on routine vaccination services.14,15 Women reported challenges in accessing maternal and child health services, including immunization, during the pandemic because of restrictions on movement due to lockdowns, lack of transportation, inability to pay for services or transportation, health worker shortages, fear of contracting COVID-19, and the mandatory use of facemasks in facilities.
A study from Shapira et al. estimates that the number of children nationally who received the third dose of the Penta vaccine decreased 9 percent between March and July 2020, while BCG coverage decreased by 4 percent in the same time period.16 However, according to WHO and UNICEF estimates, national coverage estimates of Penta1 and Penta3 have stayed the same or increased between 2019 and 2021.17 This indicates that while there were initial decreases in immunization coverage following the onset of the pandemic, Nigeria was able to prevent a significant backslide in the long-term.18
This could be attributed to efforts by the government and partners to mitigate the effects of COVID-19 on immunization service use through multiple rounds of catch-up activities, particularly in high-risk areas. For example, with the support of the Clinton Health Access Initiative (CHAI), Nigeria redesigned microplanning and data tools to accommodate infection prevention and control needs and rolled out a dashboard to visualize real-time campaign immunization coverage and reach.18
Nigeria is one of the 20 countries targeted in “The Big Catch Up,” a global initiative to reverse declines in immunization coverage seen during the COVID-19 pandemic by reaching children who missed their vaccinations during 2019–2022, restoring current vaccination coverage for the 2023 birth cohort, and using primary health care approaches to strengthen immunization systems.19 Strategies include enhancing vaccination efforts to reach ZD children through mass call backs and expanded outreach and ensuring robust newborn and default tracking. As part of this initiative, Nigeria has begun developing its Immunization Recovery Plan to reach its goal of reducing the number of ZD children by 30 percent by 2026 and by 50 percent by 2028. The plan lays out the strategies and activities to reach these goals, focusing on the 100 local government area (LGAs) with the highest number of ZD children in the first year of implementation before gradually rolling out to the remaining LGAs.20
Equity
Gavi’s 5.0 strategy to identify and reach ZD and UI children focuses on equity. To comprehensively implement Gavi’s 5.0 strategy, it is essential to examine the contexts in which ZD and UI children live.
Factors Influencing ZD Status
Figure 7 presents sociodemographic characteristics for children who did not receive Penta1, BCG, and measles vaccines. These three antigens, given at different times and different locations, can represent different immunization access barriers. Penta1 is typically used as a proxy indicator of access to routine immunization because it is given during well-child visits at 6, 10, and 14 weeks.
The measles vaccine is given first at 9 months and then again at 15 months in Nigeria, usually at primary health care facilities, and can also indicate access to routine immunization services, albeit at a later age. BCG is given at birth in Nigeria, so its coverage may better represent birth in a health facility than access to routine immunization services.
*Note: “Other” ethnic groups include those who answered “don’t know” to the question about ethnicity as well as ethnic groups that made up less than 2% of the sample.
Source: National Population Commission - NPC/Nigeria and ICF. 2019. Nigeria Demographic and Health Survey 2018. Abuja, Nigeria, and Rockville, Maryland, USA: NPC and ICF.
The data presented in Figure 7 and existing literature indicate that household wealth, the mother’s education, and where a child lives are significant predictors of whether or not a child will receive measles, BCG, or Penta1 vaccination in Nigeria.21,22 Children of mothers with lower education attainment have a greater likelihood of being ZD or UI, as do children who come from households with lower levels of wealth.21 A study by Aheto et al. found that a higher maternal education levels was positively associated with children receiving both Penta doses and a measles-containing vaccine, while higher levels of wealth were positively associated with a child receiving Penta1 and the measles vaccine.
Figure 7 also shows that children who are of the Fulani and Hausa ethnic group have lower rates of vaccination compared to other ethnic groups in Nigeria. This is supported by studies by Aheto et al., which found that children born to Igbo mothers were more likely to receive Penta1 than those born to Hausa/Fulani mothers. Afolabi et al. similarly found that Hausa/Fulani children were less likely to be vaccinated than Yoruba children.23,24 Vaccine hesitancy and mistrust, as well as cultural beliefs and misconceptions, are known barriers to providing immunization services among the Hausa and Fulani, who primarily reside in northern Nigeria.25,26,27,28,29 Additionally, the Fulani are predominantly nomadic pastoralists, and they often lack access to routine primary health care services, including immunization, and face challenges such as long distances to health facilities, limited income, and overall limited engagement with the health system.30,31,32 The Hausa and Fulani are also predominantly Muslim, who also have lower rates of immunization coverage in Nigeria compared to other religious groups. Several studies have explored the role of religion as a predictor of vaccination status in Nigeria and found that children of Muslim women are less likely to have been vaccinated, which could be due to religious objection to immunization but also presents an opportunity to engage community and religious leaders to reach ZD children in these communities.23,33,34,35
Figure 8. Number of ZD Children by District
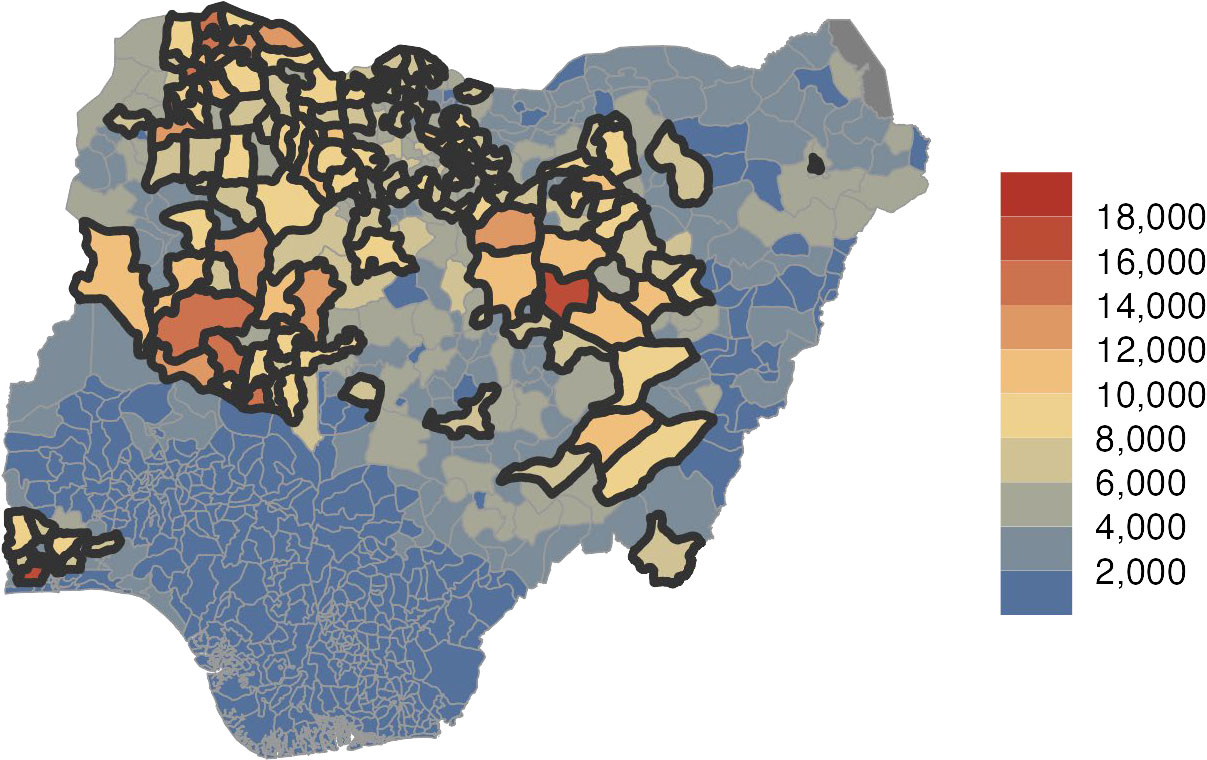
Source: IHME 2021 data cited in Gavi, Measurement and Strategic Information. 2023. “Nigeria Zero Dose Analysis.”
As the map above shows, most ZD children are located in the northern part of the country, particularly the northwest (Sokoto state), as well as around Bauchi and Kano.12 Based on IHME estimates, half of ZD children live in just 16 percent of Nigeria’s districts, outlined in black in Figure 8. The role that geographic location plays as a determinant of immunization status in Nigeria has been well documented in the literature. Children living in rural areas are more likely to be ZD compared to children in urban areas.21,36 There are also wide variations in immunization coverage by region, with the North having higher levels of ZD children and lower immunization coverage compared to the South.21,36,37 Nigeria has been found to have some of the highest levels of geographic inequity for immunization coverage in the world.5,22 For example, the district with the lowest estimated DPT1 coverage in Nigeria was Wurno, Sokoto (in the North) with only 5 percent of children receiving the vaccine, while Surulere, Lagos (in the South) had the highest coverage rate of 91 percent.5 Mosser et al. identified this as the largest absolute subnational disparity in DPT1 coverage among 49 countries in Africa. Some of this is a result of the effects of conflict and climate change on immunization access and use in Northern Nigeria, which will be described later in this report. While Northern Nigeria has a higher overall prevalence of children who are ZD, there are some areas in Southern Nigeria that also have a high prevalence of ZD children.37 According to 2021 UNICEF estimates, Alimosho LGA in Lagos State had the highest absolute number of ZD children in Nigeria, with more than 35,000 unvaccinated children.4
Health Systems
Nigeria has a pluralistic health care system, comprising public and private health sectors, as well as modern and traditional providers. The public sector is managed by the federal government, state governments, and local governments, which oversee the provision of tertiary, secondary, and primary health care services, respectively.38 Figure 9 shows that overall expenditure on health care, including government spending, has fluctuated in Nigeria over the last 20 years, increasing from $54 per capita to $96 between 2005 and 2020 and then decreasing to $70 per capita. The percentage of GDP spent on health care has decreased slightly from almost 4.5 percent in 2005 to just above 3 percent in 2020.39
Source: World Health Organization. 2022. “Global Health Expenditure Database-2022 Release.” January 24, 2022.
Compared to its neighboring countries in West Africa, Nigeria spends the most per capita on healthcare, $12 more than the next country, Cameroon, which spends $58 per capita (Figure 10).39
Source: WHO Global Health Expenditure Database. Health Expenditure Profiles.
However, a better predictor of high immunization coverage is higher levels of government spending as a proportion of total spending on health care alongside low out-of-pocket spending.40 This is because greater government investment in programs, like routine immunization, and lower out-of-pocket costs for immunization make it more accessible to children from the poorest households and their families.41 Because government spending as a proportion of total spending has decreased from 26 percent in 2005 to 15 percent in 2020, out-of-pocket spending as a proportion of total spending has simultaneously increased from 66 percent to 75 percent in the same time period (Figure 11).39 This stagnation in government spending and increase in out-of-pocket spending over the past twenty years aligns with trends seen in other lower-middle income countries globally.42
Source: WHO Global Health Expenditure Database. Health Expenditure Profiles.
Immunization Financing
Immunization is one of the most important and cost-effective public health interventions. According to one study, for every US$1 spent on immunization between 2011 and 2020, there was an average return of up to US$26 dollars across a child’s lifetime.43 In 2022, Nigeria spent approximately $177.5 million on routine immunization, including vaccines, of which 55 percent was financed by the government and 45 percent by external funders.44
Donor Support
Although Nigeria is one of Gavi’s largest recipients and Gavi is the country’s largest source of external financing for immunization, Nigeria is expected to graduate from Gavi support by 2028 after exceeding its eligibility threshold.45 Nigeria has developed a national strategy (Nigeria’s Strategy for Immunization and PHC System Strengthening [NSIPSS]) to guide its transition to self-financing.3 The NSIPSS and its complementary 2021-2024 NSIPSS 2.0 outline strategies for increasing the government’s financial commitment to immunization programming on an annual basis by strengthening financial management and identifying financing approaches to fund vaccine, operational, and system costs.3,46 In 2018, Gavi provided more than US$52 million in immunization programming support, largely to fund new and under-used vaccine support for the pneumococcal conjugate and IPV vaccines, as well as for yellow fever campaigns and measles follow-up campaigns (Figure 12).
Source: Gavi, the Vaccine Alliance Disbursement Data, 2022.
In addition to Gavi, important development partners for immunization in Nigeria include the World Bank, UNICEF, WHO, Bill & Melinda Gates Foundation, United States Agency for International Development (USAID), Centers for Disease Control and Prevention (CDC), Dangote Foundation, and the U.K. Foreign, Commonwealth and Development Office (FCDO).47
The National Primary Health Care Agency (NPHCDA), a parastatal agency within the Federal Ministry of Health (FMOH), is the main government organization responsible for driving Nigeria’s immunization policy and central coordination.46,3 There are six departments within it, including the Disease Control and Immunization department that works with development partners to provide oversight and support to supplementary immunization activities, national campaigns, and community engagement activities. The Interagency Coordination Committee (ICC), chaired by the FMOH, is the primary coordinating and decision-making body for polio eradication, routine immunization, and non-polio disease control initiatives. Its members include representatives from the FMOH, NPHCDA, LGAs, and development partners. The Core Group, chaired by the executive director of the NPHCDA, provides technical support to the ICC and oversees the planning and implementation of all immunization activities ongoing in the country. It reviews inputs from the National Emergency Routine Immunization Coordination Center (NERICC) and other working groups and provides supervisory oversight on behalf of the ICC. The NERICC, established in 2017, supports states to address immunization coverage inequities, with state and LGA-level centers also being rolled out as key coordinating mechanisms for immunization planning and monitoring in the lowest performing states.46,3
National Policies and Action Plans
The NSIPSS is the government’s primary document for outlining immunization-related priorities. The NSIPSS was developed for the period of 2018-2028, originally as part of the Gavi transition plan that started in 2017, and outlines Nigeria’s immunization programming and priorities.
The strategy describes recent immunization achievements including improvements in vaccine supply chain at the LGA level, strengthened financial management of the NPHCDA, and the establishment of the NERICC to improve routine immunization in the 18 states with the lowest coverage rates. It also describes immunization-related gaps and challenges such as stagnant immunization coverage rates, poor government funding and financing mechanisms at the federal and state levels, weak primary health care infrastructure, inadequate and inequitable distribution of qualified human resources for health, and an inadequate drug supply and sub-optimal cold chain. National objectives set forth in the plan include attaining a national coverage rate of 80 percent for all scheduled routine antigens, outlining strategies to improve equitable immunization coverage, strengthening the primary health care system, identifying and prioritizing the resources need to reach targets, and providing frameworks to guide investments, donor transitions, and implement monitoring and evaluation strategies. The NSIPSS contains several strategies for Nigeria’s immunization program relevant to ZD programming efforts. The strategy recognizes that ZD prevalence varies by state and that states with high immunization coverage still have high populations of ZD children. Therefore, equity must be a focus alongside efforts to reach national targets. Equity will be considered in decisions on the scale and intensity of strategies, and implementation plans associated with the NSIPSS will provide details on “state differentiation.” Equity will also be a factored into the introduction of new vaccines at the state level. Other strategies include periodic intensification of routine immunization through local immunization days and other activities in LGAs with high numbers of ZD children, as well as targeted and tailored services for people living in poverty in unsuccessfully reached urban informal settlements and in areas facing security risks. The focus on ZD children in the NSIPSS signals a commitment by the government to improve immunization coverage and address equity gaps.3
A complementary and updated NSIPSS was developed for 2021–2024 to provide a three-year roadmap for strengthening immunization programming based on experiences from and progress made in the first three years of the 2018-2028 NSIPSS and to reposition the NSIPSS in the context of the COVID-19 pandemic and updated global immunization agendas (Immunization Agenda 2030 and Gavi 5.0).3 The NSIPSS 2.0 includes a revised national goal of achieving routine immunization coverage of 90 percent for all antigens in at least 90 percent of LGAs. It also includes specific objectives of reducing the number of UI children by 20 percent by 2024 based on Penta3 coverage and the number of ZD children by 35 percent based on Penta1 coverage. Reducing the number of ZD children is considered in all of the objectives, strategies, and activities outlined in the document. Specific strategies for improving access to and use of immunization services for ZD children and missed communities include optimized integrated reproductive, maternal, newborn child, adolescent health, and nutrition (RMNCAH+N) and immunization sessions; a geospatial microplanning toolkit; and an integrated medical outreach program. The NSIPSS 2.0 also considers the country’s ZD reduction strategy and specifically mentions interventions to reach ZD children in humanitarian assistance contexts, including those in areas affected by conflict.
More generally, the inclusion of immunization activities in national strategy and policy documents indicates the government’s commitment to reduce vaccine preventable disease nationally. Table 3 summarizes key government documents that address the importance of immunization and outline specific activities and targets.
Table 3. National Policy and Strategy Documents Relevant to Immunization
| Policy/Legislation | Year/s | Summary |
|---|---|---|
| Nigeria Strategy for Immunisation and PHC System Strengthening (NSIPSS) | 2018–2028 | The government’s 10-year plan to improve and sustain immunization coverage and strengthen PHC service delivery. It also includes Nigeria’s plan to transition the financial ownership of the immunization and PHC system in line with its graduation from Gavi support. The plan also establishes immunization objectives, including increasing the national coverage of Penta3 to 84 percent, and strategies for system improvement ranging from leadership and accountability to data systems. |
| Nigeria Strategy for Immunisation and PHC System Strengthening Version 2.0 (NSIPSS 2.0) | 2021–2024 | The NSIPSS 2.0 is a companion document to the 2018-2028 NSIPSS that provides a short-term, three-year roadmap for reducing the number of ZD children and optimizing RI in Nigeria based on the first three years of 2018-2028 NSIPSS implementation and shifts in the local and global immunization agenda, particularly following the COVID-19 pandemic. It presents a new target of at least 90 percent coverage for all antigens in the country 2024, as well as updated objectives related to key health system functions, such as leadership and governance and service delivery. |
| Second National Strategic Health Development Plan (NSHDP II) | 2018–2022 | The NSHDP II is the Government of Nigeria’s comprehensive plan for health service delivery and systems strengthening. The plan builds upon the successes and challenges of NSHDP I (2010–2015) and aims to achieve universal health coverage. It includes strategic objectives and interventions for 15 priority areas organized under four strategic pillars. Several of these areas address immunization, including child health services and communicable diseases. |
| Nigerian Vaccine Policy | 2021 | Nigeria’s first ever vaccine policy has the overall goal of encouraging the local production of vaccine to ensure self-sufficiency in vaccine availability. Developed by the Department of Food and Drug Services as a result of the COVID-19 pandemic, the policy details the objectives, targets, and implementation strategies to achieve local vaccine production and ownership of the vaccine supply chain. |
| National Health Policy | 2016 | Following policies developed in 1988 and 2004, the 2016 National Health Policy provides a framework to operationalize the National Health Act to enable the country to attain universal health coverage. It details the goals, objectives, and initiatives needed to strengthen the health system, particularly focusing on PHC and including interventions related to immunization and vaccine-preventable diseases. |
| National Health Act | 2014 | The National Health Act serves as the legal framework for the regulation and management of the health system in Nigeria. It sets standards and regulations for health care, including its basic organization. The Act also formally establishes the Basic Health Care Provision Fund to be used to provide a basic minimum package of health services, essential drugs and vaccines, facility and equipment maintenance, and human resources for health. |
| Minimum Standards for Primary Health Care in Nigeria | 2015 | This document, developed by the National Primary Health Care Development Agency, formally establishes the standards for PHC to enable the management of health services and improve quality of care. It includes guidelines on health infrastructure, human resources for health, and service provision for facilities at the LGA level, including which providers can administer immunizations and support immunization activities. |
| Primary Health Care under One Roof Policy | 2011 | The policy drives PHC implementation in Nigeria by providing a framework for integrating all PHC services under one authority and single management body. It formally mandates states to establish State Primary Health Care Boards (or Agencies) who are responsible for managing PHC, as well as LGA Health Authority Management Teams and Advisory Committees. |
Human Resources for Health
Adequate human resources are essential for all health care services, including immunization services. However, immunization programs require a range of staff, including clinicians, supply chain professionals, logisticians, cold chain technicians, and data entry staff. Mid-level health care professionals, including nurses, midwives, and community health extension workers (CHEWs), are the main providers of immunization services in Nigeria.48,46,49 Although Nigeria has one of the largest pools of human resources for health in the region, it still faces a chronic shortage of health workers and unequal distribution particularly in the North and in rural areas.3,38 The shortage of trained health workers to provide immunization services has been reported as a key factor affecting vaccine availability and uptake.50,51,52 Data from the WHO National Health Workforce Accounts database indicate that between 2016 and 2021, the ratio of nursing and midwifery personnel decreased from 9.81 and 7.49 per 10,000 people to 9.45 and 6.18 per 10,000 people, respectively.53 Data on the number of CHEWs is limited and varying, with government figures from 2012 estimating 42,938 workers while the WHO reported only 7,912 in 2021.38,52 The 10-year NSIPSS includes a number of strategies to build a robust health workforce, including instituting a routing human resources for health assessment, improving both the number of accredited training institutions and the curriculums they use, rolling out task-shifting initiatives, and revising training packages to include junior community health workers.3
Health Management Information System Structure and Disaggregation (DHIS2), Data Availability and Use
Nigeria operationalized its national health management information system in 1999, which was then configured to DHIS2 in 2010.54,55 In 2014, partners supported the FMOH and NPHCDA to develop a routine immunization module that collects data on vaccine administration and management from the health facility level. Routine immunization data was incorporated into DHIS2 at this time.
Data from the facility level are collected via three paper-based summary forms, which are collated every month by LGA staff who enter the data into DHIS2 (Figure 13).56 DHIS2 automatically calculates 21 indicators using the raw data and displays them on a dashboard so immunization officials at the national, state, and LGA levels can monitor EPI performance and process. Indicators include information on data reporting, coverage and drop-out rates, vaccination sessions, supervision, vaccine logistics, cold chain functionality, and funding disbursed to health facilities. Roll out of DHIS2 at the state level was completed in 2017, and by July 2019, more than 80 percent of LGAs were reporting on all four data sources.54 A separate pilot study in Kano, the first state to deploy the immunization module in DHIS2, found that following implementation, the percentage of LGAs (44 total) reporting data in a timely manner increased from 67 to 88 percent, and the percentage of LGAs with complete monthly routine data increased from 70 to 87 percent.57
An analysis of RMNCH indicators in DHIS2 found the overall expected monthly facility reports was 81 percent in 2021 while only 27 percent of districts had facility reports that were at least 90 percent complete. Another analysis of routine immunization data in DHIS2 reported a completeness rate of 93 percent in December 2022.58 However, no comprehensive national-level data quality assessments of DHIS2 data, including immunization data, were identified in the literature. Several studies assessing the quality of immunization data at the state and LGA levels have found that data quality continues to be a persistent issue at the sub-national level and identified various challenges, including lack of training on reporting tools for health workers, infrequent and inadequate supervision, and heavy workloads.59,60,61,62
Figure 13. DHIS2 Reporting System in Nigeria
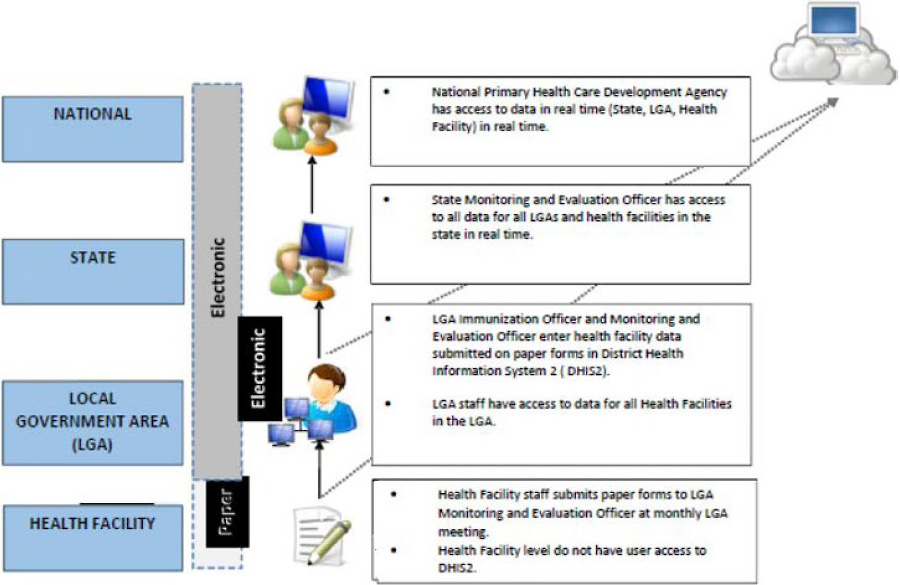
Source: Tchoualeu, Dieula Delissaint, Hashim Elzein Elmousaad, Lynda Uju Osadebe, Oluwasegun Joel Adegoke, Chimeremma Nnadi, et al. “Use of a district health information system 2 routine immunization dashboard for immunization program monitoring and decision making, Kano State, Nigeria.” The Pan African Medical Journal 40, Suppl 1 (November 12, 2021): 2. doi:10.11604/pamj.supp.2021.40.1.17313.
Several initiatives have been implemented to strengthen the HMIS as well as immunization data. In 2017, the country began rolling out a system that integrates immunization logistics data, including vaccine stock data and cold-chain equipment status, into DHIS2 so that this information can be triangulated with service delivery data.56 The NSIPSS also details efforts to improve methods for determining the denominator of immunization coverage rates by using national GIS mapping and household enumeration during microplanning.3 The 2020 Multi Stakeholder Dialogue Report from Gavi reported that these approaches had been piloted in a few LGAs.
Immunization Supply Chain and Commodities
Inadequate drug supply and sub-optimal cold chain continue to be challenges in the delivery of immunization services and is a key area of focus in the NSIPSS and the National Vaccine Policy.3,63 The Department of Logistics and Health Commodities is responsible for managing the supply chain and coordinating with State Logistics Working Groups, Logistics Management Coordination Units, and partners. Nigeria procures all of its vaccines from UNICEF and manages a five-level cold chain system with storage sites at the national, zonal, state, LGA, and facility levels. The federal government is responsible for the national strategic cold store and for transporting vaccines to the zonal and state stores, while the states and LGAs are responsible for getting vaccines to end users (Figure 14).46 The 2018–2028 NSIPSS proposes implementing a three-hub model with stores in Abuja, Lagos, and Kano to improve the efficiency and capacity of the distribution network.3
Figure 14. Vaccine Cold Chain System in Nigeria
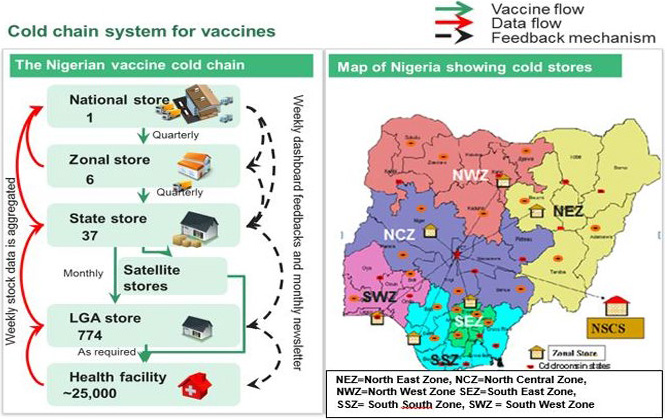
Source: Logistics Department, NPHCDA.
Vaccine unavailability, transportation challenges from cold storage at the LGA to facilities, and inadequate power supply to maintain cold storage at the facility level have been cited as challenges in immunization service delivery.49 Ensuring a stable vaccine supply chain is critical to improving immunization coverage. A study by Gooding et al. found that stockouts significantly affected the number of children immunized for all antigens included in the analysis (polio, BCG, measles, yellow fever, Penta, pneumococcal conjugate, and hepatitis B). For example, a stockout of the polio vaccine resulted in 226 fewer children receiving the vaccine in the same month. Furthermore, a stockout in one month resulted in fewer children being vaccinated in the following months for some antigens.64
Since 2016, the NPHCDA has established long-term contracts with third party logistics providers for a vaccine transport system from the national to state level and has proposed a scale-up of its “Push Plus” system that provides direct delivery to cold chain-equipped facilities to address challenges at the last mile.3 A preliminary assessment of this system in Kano State found that there was an increase in stock adequacy from 54 percent to 68 percent and a decrease in stock-out rates from 41 percent to 10 percent following 20 months of implementation.65 Another study also found that the new push system had improved access to immunization by eliminating the need for facility workers to visit vaccine storage facilities and helping to ensure the facility has a consistent supply of vaccines.28
Community Health Structure and Role in Routine Immunization
Nigeria does not have a formal policy or strategy on community health care, but various policies focused on primary health care provide strategies and frameworks for community health including its role in immunization service delivery. The LGAs are responsible for the delivery of primary health care and coordinate with Ward Development Committees (WDC) and Village Development Committees (VDC) to provide the community with links to health posts, primary health clinics, and primary health centers. These committees also supervise the CHEWs, community health officers (CHOs), community resource persons (CORPs), and junior community health extension workers (JCHEWs). CHOs, CHEWs, and JCHEWs are all salaried providers at the lowest level of the primary health care system and receive formal training. CORPs is a general term that encompasses informal community health providers often supported by NGOs.66
According to the FMOH’s Minimum Standards for Primary Health Care, CHOs, CHEWs, and JCHEWs can all identify eligible pregnant women and children for immunization, provide routine immunization, participate in immunization campaigns, and assist in the management of adverse effects and identification of acute flaccid paralysis.47
Immunization Program Details
Nigeria’s National Program on Immunization was first established in 1978 and then later merged with the NPHCDA in 2007 so that it was fully integrated with the primary health care system. Immunization services are provided at health facilities, by CHEWs through weekly outreach services conducted within 5 to 10 km from an assigned health facility, and monthly mobile services that target populations more than 10 km away from a facility.
The NPHCDA is responsible for national-level policy, planning, and regulation while the state ministries of health, mainly the state health care development agencies (SPHCDAs), oversee the implementation of primary health care and oversee LGAs who are primarily responsible for immunization service delivery (Figure 15). The local governments are supported by ward and village development committees, although the functionality of these committees is not standard and varies by state.46 For example, a study on immunization use in Remo-North LGA in Ogun State found that a development committee in one ward had been promoting community linkages with the health facility and immunization services while the committee in a nearby ward had been defunct due to political disagreements for several years.49
Figure 15. Health System in Nigeria
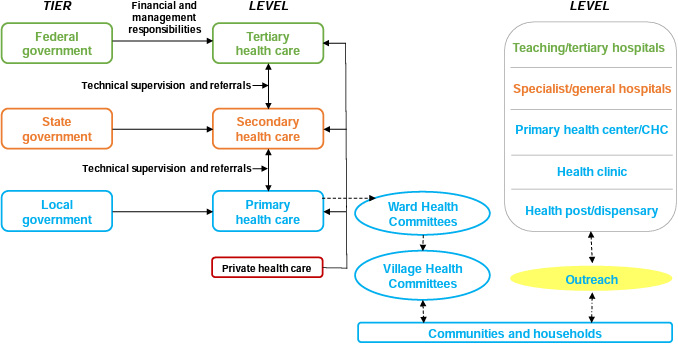
Source: Adapted from Ojo, Jimoh, and Nwali (2009); Saleh et al, 2017.
Environmental Context
Climate Change
Nigeria is no exception to the increasing risk that climate change poses to public health worldwide. Studies have documented the impact of climate change in Nigeria, including rising temperatures, variable rainfall, increased flooding, sea level rise, and drought.67 The effects of climate change vary across the country, with the North being considered the most vulnerable, as well as the Niger Delta Region in the South.66,68 While the impact of climate change on health challenges in Nigeria has been studied, its impact on immunization services is not well understood.69,70,71 However, it is known that climate change plays a role in the incidence of vaccine-preventable diseases, such as cholera, meningitis, pneumonia, and yellow fever.72,73,74,75
The interaction between climate change, conflict, and population displacement could exacerbate further gaps in immunization coverage, with northern Nigeria experiencing the worst of these consequences. In addition to violence from insurgencies, forced migration and displacement because of drought and desertification has resulted in social conflict, particularly between farming and pastoralist communities.76 Targeted and tailored immunization service delivery will be critical to reaching these populations, as happened in Borno where an emergency cholera vaccine campaign took place following flooding in an area with a large number of camps for internally displaced people escaping Boko Haram violence.77
Conflict
According to the International Organization for Migration, there are almost 2.4 million internally displace persons (IDPs) in Nigeria, mainly in the northeast. Borno state has more than half of the country’s displaced population, an estimated 1.87 million people. Almost all (95 percent) of IDPs report insurgency as the main reason for their displacement, while the other 5 percent identify communal clashes as their primary reason.78 Overall, armed conflict and violent insurgency in Northern Nigeria has caused the displacement of more than 3.6 million people as of 2022.77
Boko Haram first emerged in the early 2000s, with violence escalating into a full-blow conflict with Nigerian military forces in the Northeast in 2009.79 Since then, Boko Haram has splintered into two main factions, the Islamic State West Africa Province (ISWAP) and Jama’atu Ahlis Sunna Lidda’awati-Jihad (JAS).80 The scale of violence has fluctuated but continued with attacks being reported this year in Borno.78,81 The epicenter of the insurgency is in the states of Borno, Adamawa, and Yobe. There have been reports of crime and kidnapping in the northwest, violence between farmers and pastoralists in the middle belt, and separatist movements in the southeast.78
In addition to violent insurgency, clashes between nomadic pastoralists, who are mainly of the Fulani ethnic group, and farmers have led to widespread conflict in some areas of Nigeria. This conflict over land is further fueled by desertification and scarcity of fresh water as a result of climate change.82 Violent attacks in Benue and Nasarawa states resulted in the displacement of approximately 170,000 people and severely disrupted health services, including immunization service delivery.83 While supplementary immunization activities have expanded access to vaccination among hard-to-reach people, including areas affected by herdsman-farmer conflict, there is limited knowledge of how this conflict has affected immunization service delivery and coverage.82,84
Overall, conflict has severely disrupted health service delivery, with some 40 percent of health facilities being damaged or destroyed. In the states of Borno, Adamawa, and Yobe, an estimated 31 percent of health facilities are no longer functional, limiting access to health services in an area that already has some of the worst health indicators in the country.78 Northern Nigeria has some of the lowest immunization coverage rates in the country and in Africa, which could be attributed in part to the violence seen in the region. Wigley et al. estimate that 34 percent of children in conflict areas of Nigeria are unvaccinated.85 A study from Ojeleke et al. in 2020 found that children living in Northern Nigeria within 5 km of a conflict event had 24 percent lower odds of being vaccinated and 37 percent lower odds if they lived within 10 km of conflict compared to children not living near a conflict event.6 A similar study focusing on Adamawa, Borno, and Yobe states found that if a conflict event occurred in the same month as the child was born, there odds of being immunized were 47 percent lower for any vaccination, 45 percent lower for BCG vaccination, and 48 percent lower for DPT1 vaccination.86 Several studies have documented the challenges of delivering immunization services to children living in areas experiencing conflict, contributing to the low immunization coverage in these areas.87,88,89 Furthermore, conflict can limit the ability to collect quality data, potentially resulting in inaccurate estimates of immunization coverage.90 Both the DHS and MICS noted that they could not collect data from several LGAs in Borno state because of insecurity, affecting the representativeness of the data from Borno and possibly leading to over estimation of immunization coverage.89,2
Areas for Further Inquiry
While this landscape attempts to present a holistic picture of the immunization context in Nigeria, there are gaps in information that will be critical to fill to effectively and sustainably reach ZD and UI and missed communities. Table 4 summarizes gaps that emerged while developing this landscape and the rationale for additional inquiry. The development of the ZD learning agenda with stakeholders in Nigeria will provide an opportunity to prioritize these and other areas of inquiry going forward.
Table 4. Information Gaps Relevant to ZD Children in Nigeria
| Gap | Rationale |
|---|---|
| Information about barriers to immunization in urban areas. | The current evidence on the factors contributing to ZD and UI status in urban areas is limited. The LGA in Nigeria with the most ZD children is an urban area in Lagos State, so understanding the specific barriers experienced by this and similar populations with high absolute numbers of ZD children will be critical to reaching them with immunization services. |
| Robust evidence and testing on the most effective programmatic approaches to reach ZD communities and children. | Although evidence exists on the overarching barriers to immunization in Nigeria, there is less information on the most effective programmatic approaches to reaching ZD children. Additional operations research on interventions to overcome barriers is needed to address challenges and design effective programs to provide tailored immunization services for different contexts, including conflict zones, nomadic populations, and rural areas. |
| Comprehensive, national-level evidence regarding data quality of administrative data sources for accurately calculating immunization coverage. | Current evidence on data quality is mainly limited to assessments conducted at the state and LGA-level. While this is important to developing local strategies, having a comprehensive national-level landscape of data quality is fundamental to guiding national-level strategies, decision-making, and prioritization of resources related to ZD children. |
| Further understanding of how conflict between herdsmen/pastoralists and farmers has affected immunization coverage, particularly in Northern Nigeria. | Current evidence on this is limited. While it is known that herdsmen/pastoralists, such as the Fulani, have particularly low rates of immunization and that conflict, mainly from insurgencies, has impacted immunization access in Nigeria, there is limited understanding of the impact of conflict among these two groups on immunization coverage and service delivery in affected areas. In depth, qualitative inquiry regarding the intersecting and nuanced barriers experienced by marginalized populations is important to develop tailored and context-specific strategies to reach ZD and UI children. |
| Information about additional environmental factors that impact immunization coverage in the country. | The current evidence on the direct effects of climate change on immunization is limited for Nigeria. As the effects of climate change increase, it will be critical to know its impact on both the demand and supply of immunization services to ensure that immunization systems are prepared and resilient. |
Immunization Partners and Zero Dose Efforts
Table 5 below shows a list of immunization stakeholders engaged in ZD efforts in Nigeria. The content will be expanded in future iterations of the landscape through a series of planned key informant interviews with stakeholders at national and subnational levels.
Table 5. List of Preliminary Immunization Stakeholders in Nigeria
| Sl. No. | Organization/Entity | Category | Geographic coverage | Dates of work | Funder | Description of work |
|---|---|---|---|---|---|---|
| 1 | National Primary Health Care Development Board (NPHCDA) | Government | National | 1992–present | Federal Ministry of Health | Parastatal agency mandated to develop national primary health care policy, support planning and management of primary health care services, and provide oversight of the national immunization program. |
| 2 | State Primary Health Care Development Agencies (SPHCDA) | Government | State (all 36 and FCT) | 2012–present | State Ministries of Health | Oversees the implementation of primary health care at the state-level, with oversight from the NPHCDA. |
| 3 | National Emergency Routine Immunization Coordination Centre (NERICC) | Government | National | 2017–present | NPHCDA | Strengthens routine immunization in the states and LGAs with the lowest performing immunization coverage. |
| 4 | World Bank | Funder | International | 1958–present | The International Development Association (IDA) | Supports Nigeria’s development journey including poverty reduction and economic growth acceleration. |
| 5 | Gavi | Funder | International | 2001–present | Gavi | Funds initiatives to promote vaccination of children against deadly and debilitating infectious diseases. |
| 6 | Bill and Melinda Gates Foundation | Funder | International | 2012–present | Gates Foundation | Funds programs to fight poverty, disease, and inequity In Nigeria to reduce preventable deaths. |
| 7 | United Nations International Children’s Emergency Fund (UNICEF) | Funder/Technical Assistance | International | 1952–present | UNICEF | Supports the country’s efforts to address the needs of the most vulnerable children, including working with all levels of government to provide immunization services. |
| 8 | United States Agency for International Development (USAID) | Funder/Technical Assistance | International | 1960–present | U.S. Government | Strengthens Nigeria’s capacity to deliver MNCH services, including immunization delivery. |
| 9 | World Health Organization (WHO) | Funder/Technical Assistance | International | 1960–present | WHO | Provides technical advice and support to improve the health and development of Nigerians, including monitoring and assessing trends in health indicators. |
| 10 | Rotary International | Funder/Technical Assistance | International | 1961–present | Public donations and contributions | Global service organization that brings together different leaders and communities to improve the wellbeing of Nigerians. |
| 11 | Clinton Health Access Initiative (CHAI) | Funder/Technical Assistance | International | 2007–present | Gates Foundation, among others | Reduces the burden of disease in Nigeria by strengthening the government and private sector to sustain high-quality health systems. |
| 12 | MOMENTUM Routine Immunization Transformation and Equity (MRITE) | Technical Assistance | Bayelsa, Edo, Imo, Jigawa, Lagos | 2022–present | USAID | Works to build the country’s capacity to identify and overcome barriers to reaching ZD and UI children and other integrated health services. |
| 13 | Global Polio Eradication Initiative (GPEI) | Technical Assistance | International | 1988–present | WHO, among others | Supports the country’s progress in protecting Nigerians from polio and eradicating the disease worldwide. |
| 14 | Syndani | Technical Assistance | National | 2020–present | Gates Foundation, among others | Supports the NPHCDA in data analysis and reporting. |
| 15 | Save the Children | Technical Assistance | National | 2001–present | Various | Strengthens immunization programming through national, sub-national, and community-level efforts, including advocacy. |
| 16 | The Africa Field Epidemiology Network (AFENET) | Research and Implementation | National | 2005–present | N/A | Works with ministries of health and other platforms to improve health outcomes in Nigeria by building capacity for public health preparedness. |
| 17 | Solina Centre for International Development and Research | Research and Implementation | National | 2010–present | Gates Foundation, among others | Works to improve health outcomes in Nigeria by providing research, capacity building, and health advisory services to governments and other partners. |
| 18 | The Christian Health Association of Nigeria | Research and Implementation | Bauchi, Borno, Kaduna, Plateau, Sokoto | 2023–present | Gavi | Facilitates research related to ZD children and supports the adaptation of immunization services. |
| 19 | London School of Hygiene & Tropical Medicine (LSHTM) | Research and Implementation | National | N/A | Unknown | Conducts research and supports locally-led research to improve service delivery and strengthen public health approaches. |
| 20 | Global Health Advocacy Incubator | Technical Assistance/ Advocacy | National | 2023 | Gavi | Supports civil society organizations to secure social and political will for equitable and sustainable financing for immunization and primary health care; works towards increasing immunization coverage and reducing the number of ZD children; and ensures efficient use and allocation of domestic resources and international donor funds for primary health care and immunization service delivery. |
Relevant Resources
Below are several relevant resources related to health and immunization in Nigeria, including surveys, data, reports, and databases.
Surveys
- Nigeria Demographic and Health Survey 2013
- Nigeria 2016–2017 Multiple Indicator Cluster Survey
- Nigeria Demographic and Health Survey 2018
- Nigeria 2021 Multiple Indicator Cluster Survey/National Immunization Coverage Survey Report
Immunization and Health Data
Program Reports, National Strategies, and Databases
- Nigeria Strategy for Immunisation and PHC System Strengthening [NSIPSS] 2018–2028
- Second National Strategic Health Development Plan 2018–2022
- Nigeria Vaccine Policy, 1st Edition 2021
- Global Health Expenditure Database, 2022 Release
Anticipated Work/Publications
References
1 National Population Commission (NPC/Nigeria) and ICF. “Nigeria Demographic and Health Survey 2018 - Final Report,” October 1, 2019.
2 UNICEF. 2021 Multiple Indicator Cluster Survey/National Immunization Coverage Survey Report | UNICEF Nigeria. 2022.
3 National Primary Health Care Development Agency (NPHCDA). Nigeria Strategy for Immunization and PHC System Strengthening Version 2.0 (2021-2024). A Companion Document to Nigeria Strategy for Immunization and PHC System Strengthening [NSIPSS 2018-2028]. 2021. Unpublished.
4 Gavi. Comprehensive Multi-Year Plan Nigeria 2018-2028. Nigeria Strategy for Immunisation and PHC System Strengthening (NSIPSS). April 18, 2018.
5 World Health Organization/UNICEF Estimates of National Immunization Coverage (WUENIC)—2022 estimates. (2022). WHO Immunization Data Portal.
6 Mosser, Jonathan F., William Gagne-Maynard, Puja C. Rao, Aaron Osgood-Zimmerman, Nancy Fullman, Nicholas Graetz, Roy Burstein, et al. “Mapping Diphtheria-Pertussis-Tetanus Vaccine Coverage in Africa, 2000–2016: A Spatial and Temporal Modelling Study.” The Lancet 393, no. 10183 (May 4, 2019): 1843–55.
7 Ojeleke, Olabayo, Wim Groot, Isaac Bonuedi, and Milena Pavlova. “The Impact of Armed Conflicts on Health-Care Utilization in Northern Nigeria: A Difference-in-Differences Analysis.” World Medical & Health Policy 14, no. 4 (2022): 624–64.
8 World Bank Open Data. “World Bank Open Data.” Accessed August 2, 2023.
9 World Health Organization. “Child Mortality (under 5 Years) Fact Sheet,” January 28, 2022.
10 IGME. “CME Info - Child Mortality Estimates.” UN Inter-agency Group for Child Mortality Estimation. Accessed August 2, 2023.
11 Institute for Health Metrics and Evaluation. “GBD Results.” Accessed August 2, 2023.
12 Gavi MEL Team. “Nigeria Zero-Dose Analysis.” Unpublished. September 2022.
13 Burton, Anthony, Roeland Monasch, Barbara Lautenbach, Marta Gacic-Dobo, Maryanne Neill, Rouslan Karimov, Lara Wolfson, Gareth Jones, and Maureen Birmingham. “WHO and UNICEF Estimates of National Infant Immunization Coverage: Methods and Processes.” Bulletin of the World Health Organization 87, no. 7 (July 2009): 535–41.
14 Balogun, Mobolanle, Aduragbemi Banke-Thomas, Adekemi Sekoni, Godfred O. Boateng, Victoria Yesufu, Ololade Wright, Osinachi Ubani, Akin Abayomi, Bosede B. Afolabi, and Folasade Ogunsola. “Challenges in Access and Satisfaction with Reproductive, Maternal, Newborn and Child Health Services in Nigeria during the COVID-19 Pandemic: A Cross-Sectional Survey.” PloS One 16, no. 5 (2021): e0251382.
15 Akaba, Godwin O, Osasuyi Dirisu, Kehinde S. Okunade, Eseoghene Adams, Jane Ohioghame, Obioma O. Obikeze, Emmanuel Izuka, Maryam Sulieman, and Michael Edeh. “Barriers and Facilitators of Access to Maternal, Newborn and Child Health Services during the First Wave of COVID-19 Pandemic in Nigeria: Findings from a Qualitative Study.” BMC Health Services Research 22 (May 6, 2022): 611.
16 Shapira, Gil, Tashrik Ahmed, Salomé Henriette Paulette Drouard, Pablo Amor Fernandez, Eeshani Kandpal, Charles Nzelu, Chea Sanford Wesseh, et al. “Disruptions in Maternal and Child Health Service Utilization during COVID-19: Analysis from Eight Sub-Saharan African Countries.” Health Policy and Planning 36, no. 7 (August 12, 2021): 1140–51.
17 World Health Organization. “WHO Immunization Data Portal.” Accessed August 2, 2023.
18 Athiyaman, Anithasree, Tosin Ajayi, Faith Mutuku, Fredrick Luwaga, Sarah Bryer, Omotayo Giwa, Shadrack Mngemane, Nnang Nadege Edwige, and Leslie Berman. “Recovering from the Unprecedented Backsliding in Immunization Coverage: Learnings from Country Programming in Five Countries through the Past Two Years of COVID-19 Pandemic Disruptions.” Vaccines 11, no. 2 (February 7, 2023): 375.
19 “The Big Catch-Up: An Essential Immunization Recovery Plan for 2023 and Beyond.” Accessed August 2, 2023.
20 Federal Ministry of Health. “Nigeria Immunization Recovery Plan (2023–2028).” Sent via personal email communication. July 13, 2023.
21 Sato, Ryoko. “Zero-Dose, Under-Immunized, and Dropout Children in Nigeria: The Trend and Its Contributing Factors over Time.” Vaccines 11, no. 1 (January 2023): 181.
22 Dimitrova, Anna, Gabriel Carrasco-Escobar, Robin Richardson, and Tarik Benmarhnia. “Essential Childhood Immunization in 43 Low- and Middle-Income Countries: Analysis of Spatial Trends and Socioeconomic Inequalities in Vaccine Coverage.” PLOS Medicine 20, no. 1 (January 17, 2023): e1004166.
23 Aheto, Justice Moses K., Oliver Pannell, Winfred Dotse-Gborgbortsi, Mary K. Trimner, Andrew J. Tatem, Dale A. Rhoda, Felicity T. Cutts, and C. Edson Utazi. “Multilevel Analysis of Predictors of Multiple Indicators of Childhood Vaccination in Nigeria.” PLOS ONE 17, no. 5 (May 25, 2022): e0269066.
24 Afolabi, Rotimi Felix, Mobolaji M. Salawu, Babatunde Makinde Gbadebo, Adetokunbo T. Salawu, Adeniyi Francis Fagbamigbe, and Ayo Stephen Adebowale. “Ethnicity as a Cultural Factor Influencing Complete Vaccination among Children Aged 12-23 Months in Nigeria.” Human Vaccines & Immunotherapeutics 17, no. 7 (July 3, 2021): 2008–17.
25 Ahmad I. M., Yunusa I., Wudil A. M., Gidado Z. M., Sharif A. A., Kabara H. T.. Knowledge, Attitude, Perception and Beliefs of Parents/Care givers About Polio Immunization. International Journal of Public Health Research. Vol. 3, No. 5, January 2015, pp. 192-199.
26 “Perception of Illness and Health Seeking Behavior among Fulani in Wamakko Local Government Area of Sokoto State, Nigeria.” Accessed August 2, 2023.
27 Sato, Ryoko, and Yoshito Takasaki. “Vaccine Hesitancy and Refusal: Behavioral Evidence from Rural Northern Nigeria.” Vaccines 9, no. 9 (September 14, 2021): 1023.
28 Olaniyan, Abisola, Chinwoke Isiguzo, Saheed Agbomeji, Olubunmi Akinlade-Omeni, Belinda Ifie, and Mary Hawk. “Barriers, Facilitators, and Recommendations for Childhood Immunisation in Nigeria: Perspectives from Caregivers, Community Leaders, and Healthcare Workers.” The Pan African Medical Journal 43 (October 25, 2022): 97.
29 Ozawa, Sachiko, Chizoba Wonodi, Olufemi Babalola, Tukur Ismail, and John Bridges. “Using Best-Worst Scaling to Rank Factors Affecting Vaccination Demand in Northern Nigeria.” Vaccine 35, no. 47 (November 7, 2017): 6429–37.
30 Alarima, C. I., and F. E. Obikwelu. “Assessment of Utilization of Primary Health Care Services among Settled Fulani Agro-Pastoralists in Ogun State, Nigeria.” Agro-Science 17, no. 1 (August 2, 2018): 27–34.
31 Gidado, Saheed O., Chima Ohuabunwo, Patrick M. Nguku, Ikechukwu U. Ogbuanu, Ndadilnasiya E. Waziri, Oladayo Biya, Eric S. Wiesen, et al. “Outreach to Underserved Communities in Northern Nigeria, 2012–2013.” The Journal of Infectious Diseases 210, no. suppl_1 (November 1, 2014): S118–24.
32 Okeibunor, Joseph C, Nkechi G Onyeneho, Obioma C Nwaorgu, Ngozi I’Aronu, Ijeoma Okoye, Felicia U Iremeka, and Johannes Sommerfeld. “Prospects of Using Community Directed Intervention Strategy in Delivering Health Services among Fulani Nomads in Enugu State, Nigeria.” International Journal for Equity in Health 12 (April 8, 2013): 24.
33 Ljarotimi, Ibidolapo T., Akinola A. Fatiregun, Oluwapelumi A. Adebiyi, Olayinka S. Ilesanmi, and Olufemi Ajumobi. “Urban–Rural Differences in Immunisation Status and Associated Demographic Factors among Children 12-59 Months in a Southwestern State, Nigeria.” PLOS ONE 13, no. 11 (November 5, 2018): e0206086.
34 Costa, Janaína Calu, Ann M. Weber, Gary L. Darmstadt, Safa Abdalla, and Cesar G. Victora. “Religious Affiliation and Immunization Coverage in 15 Countries in Sub-Saharan Africa.” Vaccine 38, no. 5 (January 29, 2020): 1160–69.
35 Antai, Diddy. “Faith and Child Survival: The Role of Religion in Childhood Immunization in Nigeria.” Journal of Biosocial Science 41, no. 1 (January 2009): 57–76.
36 Wagai, John Ndegwa, Dale Rhoda, Mary Prier, Mary Kay Trimmer, Caitlin B. Clary, Joseph Oteri, Bassey Okposen, Adeyemi Adeniran, Carolina Danovaro-Holliday, and Felicity Cutts. “Implementing WHO Guidance on Conducting and Analysing Vaccination Coverage Cluster Surveys: Two Examples from Nigeria.” PLOS ONE 16, no. 2 (February 26, 2021): e0247415.
37 Utazi, C. Edson, Justice M. K. Aheto, Adelle Wigley, Natalia Tejedor-Garavito, Amy Bonnie, Christopher C. Nnanatu, John Wagai, et al. “Mapping the Distribution of Zero-Dose Children to Assess the Performance of Vaccine Delivery Strategies and Their Relationships with Measles Incidence in Nigeria.” Vaccine 41, no. 1 (January 4, 2023): 170–81.
38 Federal Ministry of Health. “Second National Strategic Health Development Plan 2018–2022.” 2018.
39 World Health Organization. “Global Health Expenditure Database.” Accessed August 2, 2023.
40 Arsenault, Catherine, Mira Johri, Arijit Nandi, José M. Mendoza Rodríguez, Peter M. Hansen, and Sam Harper. “Country-Level Predictors of Vaccination Coverage and Inequalities in Gavi-Supported Countries.” Vaccine 35, no. 18 (April 25, 2017): 2479–88.
41 Wagstaff, Adam, Patrick Hoang-Vu Eozenou, and Marc-Francois Smitz. “Out-of-Pocket Expenditures on Health: A Global Stocktake.” SSRN Scholarly Paper. Rochester, NY, April 8, 2019.
42 World Health Organization. “Global Expenditure on Health: Public Spending on the Rise?” Accessed August 2, 2023.
43 Sim, So Yoon, Elizabeth Watts, Dagna Constenla, Logan Brenzel, and Bryan N. Patenaude. “Return On Investment From Immunization Against 10 Pathogens In 94 Low- And Middle-Income Countries, 2011-30.” Health Affairs (Project Hope) 39, no. 8 (August 2020): 1343–53.
44 “WHO Immunization Data Portal.” Accessed August 2, 2023.
45 Linked Immunisation Action Network. “Transitioning from Donor Support: Lessons Learned from Nigeria’s Gavi Transition Plan Development,” June 9, 2021.
46 “Comprehensive Multi-Year Plan Nigeria 2018-2028.” Nigeria Strategy for Immunisation and PHC System Strengthening (NSIPSS). April 18, 2018.
47 World Bank. “Nigeria Immunization Financing Assessment.” Text/HTML. Accessed August 2, 2023.
48 NPHCDA. “Minimum Standards for Primary Health Care in Nigeria.” Department of Planning, Research and Statistics. 2012.
49 Eboreime, Ejemai, Seye Abimbola, and Fiammetta Bozzani. “Access to Routine Immunization: A Comparative Analysis of Supply-Side Disparities between Northern and Southern Nigeria.” PLOS ONE 10, no. 12 (December 21, 2015): e0144876.
50 Akwataghibe, Ngozi N., Elijah A. Ogunsola, Jacqueline E. W. Broerse, Oluwafemi A. Popoola, Adanna I. Agbo, and Marjolein A. Dieleman. “Exploring Factors Influencing Immunization Utilization in Nigeria—A Mixed Methods Study.” Frontiers in Public Health 7 (2019).
51 Oku, Afiong, Angela Oyo-Ita, Claire Glenton, Atle Fretheim, Glory Eteng, Heather Ames, Artur Muloliwa, et al. “Factors Affecting the Implementation of Childhood Vaccination Communication Strategies in Nigeria: A Qualitative Study.” BMC Public Health 17, no. 1 (February 15, 2017): 200.
52 Erchick, Daniel J., Asha S. George, Chukwunonso Umeh, and Chizoba Wonodi. “Understanding Internal Accountability in Nigeria’s Routine Immunization System: Perspectives From Government Officials at the National, State, and Local Levels.” International Journal of Health Policy and Management 6, no. 7 (December 10, 2016): 403–12.
53 World Health Organization. “Welcome NHWA Web Portal.” Accessed August 4, 2023.
54 Bosch-Capblanch, Xavier, N. Saric C. Njepuome, C. Guterman J. Jarrett, Maureen Curry, Angela Oyo-Ita and P. Garba E. Ogah. “Characterisation of the health information system in Nigeria.” Swiss Tropical and Public Health Institute. 2017.
55 Shuaib, Faisal, Abdullahi Bulama Garba, Emmanuel Meribole, Samuel Obasi, Adamu Sule, Chimeremma Nnadi, Ndadilnasiya Endie Waziri, et al. “Implementing the Routine Immunisation Data Module and Dashboard of DHIS2 in Nigeria, 2014–2019.” BMJ Global Health 5, no. 7 (July 1, 2020): e002203.
56 Tchoualeu, D. D., Elmousaad, H. E., Osadebe, L. U., Adegoke, O. J., Nnadi, C., Haladu, S. A., Jacenko, S. M., Davis, L. B., Bloland, P. B., & Sandhu, H. S. (2021). “Use of a district health information system 2 routine immunization dashboard for immunization program monitoring and decision making, Kano State, Nigeria.” The Pan African Medical Journal, 40(Suppl 1), 2.
57 Uba, Belinda Vernyuy, Ndadilnasiya Endie Waziri, Oluwasegun Joel Adegoke, Adekunle Akerele, Saheed Gidado, Nnamdi Usifoh, Olorunsogo Bidemi Adeoye, et al. “Pilot Implementation of a Routine Immunization Module of the District Health Information System Version 2 in Kano State, Nigeria, 2014 - 2015.” The Pan African Medical Journal 40, no. 5 (November 12, 2021).
58 Chikwado. “Nigeria Integrates Last-Mile Vaccine Supply Chain Data in DHIS2 to Improve Visibility and Use at Sub-National Levels.” DHIS2, February 28, 2023.
59 Ogbuabor, D. C., N. Ghasi, U. J. Okenwa, Chukwunweike N. Nwangwu, U. Ezenwaka, and O. Onwujekwe. “Assessing the Quality of Immunization Data from Administrative Data in Enugu State, South-East Nigeria: A Cross-Sectional Study.” Nigerian Journal of Clinical Practice 25, no. 11 (November 2022): 1864–74.
60 Bhattacharya, Antoinette Alas, Nasir Umar, Ahmed Audu, Habila Felix, Elizabeth Allen, Joanna R. M. Schellenberg, and Tanya Marchant. “Quality of Routine Facility Data for Monitoring Priority Maternal and Newborn Indicators in DHIS2: A Case Study from Gombe State, Nigeria.” PLOS ONE 14, no. 1 (January 25, 2019): e0211265.
61 Omoleke, Semeeh Akinwale, and Menberu Getachew Tadesse. “A Pilot Study of Routine Immunization Data Quality in Bunza Local Government Area: Causes and Possible Remedies.” The Pan African Medical Journal 27, no. 239 (February 8, 2017).
62 Akerele, Adekunle, Ramatu Obansa, Oluwasegun Joel Adegoke, Suleiman Haladu, Olorunsogo Bidemi Adeoye, Nnamdi Usifoh, Sulaiman Etamesor, Belinda Uba, and Ndadilnasiya Endie Waziri. “Determinants of Improved Data Consistency across Routine Immunization Data Tools for Health Facilities in Kano State, Nigeria.” The Pan African Medical Journal 36 (2020): 148.
63 Federal Ministry of Health. “Nigeria Vaccine Policy: 1st Edition.” Department of Food and Drug Services. 2021.
64 “Impact of Vaccine Stockouts on Immunization Coverage in Nigeria.” Vaccine 37, no. 35 (August 14, 2019): 5104–10.
65 Aina, Muyi, Uchenna Igbokwe, Leke Jegede, Rabiu Fagge, Adam Thompson, and Nasir Mahmoud. “Preliminary Results from Direct-to-Facility Vaccine Deliveries in Kano, Nigeria.” Vaccine, Building Next Generation Immunization Supply Chains, 35, no. 17 (April 19, 2017): 2175–82.
66 Farnham Egan, Kimberly, Kristen Devlin, and Pandit-Rajani, Tanvi. “Community Health Systems Catalog Country Profile: Nigeria.” Arlington, VA: Advancing Partners & Communities, 2017.
67 “Climate Change in Nigeria: Impacts and Responses | PreventionWeb,” November 13, 2019.
68 Okon, E.M., B.M. Falana, S.O. Solaja, S.O. Yakubu, O.O. Alabi, B.T. Okikiola, T.E. Awe, et al. “Systematic Review of Climate Change Impact Research in Nigeria: Implication for Sustainable Development.” Heliyon 7, no. 9 (September 6, 2021): e07941.
69 Raimi, Morufu Olalekan, Odubo Tonye Vivien, and Omidiji Adedoyin Oluwatoyin. “Creating the Healthiest Nation: Climate Change and Environmental Health Impacts in Nigeria: A Narrative Review.” SSRN Scholarly Paper. Rochester, NY, February 9, 2021.
70 Monday, Ilevbare Femi. “Investigating Effects of Climate Change on Health Risks in Nigeria.” In Environmental Factors Affecting Human Health. IntechOpen, 2019.
71 World Health Organization. “Health and Climate Change: Country Profile 2015: Nigeria.” December 3, 2016.
72 Oluwatimilehin, Isaac Ayo, Joseph Omojesu Akerele, Tolulope Adedoyin Oladeji, Mojisola Hannah Omogbehin, and Godwin Atai. “Assessment of the Impact of Climate Change on the Occurrences of Malaria, Pneumonia, Meningitis, and Cholera in Lokoja City, Nigeria.” Regional Sustainability 3, no. 4 (December 1, 2022): 309–18.
73 Felix, Ike. “Effects of Weather and Climatic Elements on the Incidence of Pneumonia in Kaduna South Local Government Area, North Western Nigeria.” SSRN Scholarly Paper. Rochester, NY, March 1, 2019.
74 Abaje, I. B., N. Abdullahi, and O. G. Jeje. “Climate Change and Infectious Diseases in Funtua Local Government Area of Katsina State, Nigeria.” AFRREV STECH: An International Journal of Science and Technology 5, no. 1 (February 9, 2016): 47–58.
75 Gaythorpe, Katy AM, Arran Hamlet, Laurence Cibrelus, Tini Garske, and Neil M Ferguson. “The Effect of Climate Change on Yellow Fever Disease Burden in Africa.” Edited by Alex R Cook and Eduardo Franco. ELife 9 (July 28, 2020): e55619.
76 Olagunju, T. E., S. O. Adewoye, A. O. Adewoye, and O. A. Opasola. “Climate Change Impacts on Environment: Human Displacement and Social Conflicts in Nigeria.” IOP Conference Series: Earth and Environmental Science 655, no. 1 (February 2021): 012072.
77 Ngwa, Moise Chi, Wondimagegnehu Alemu, Ifeanyi Okudo, Collins Owili, Uzoma Ugochukwu, Peter Clement, Isabelle Devaux, et al. “The Reactive Vaccination Campaign against Cholera Emergency in Camps for Internally Displaced Persons, Borno, Nigeria, 2017: A Two-Stage Cluster Survey.” BMJ Global Health 5, no. 6 (June 29, 2020): e002431.
78 International Organization for Migration. “Nigeria | Displacement Tracking Matrix.” Global Data Institute. Accessed August 2, 2023.
79 UN Office for the Coordination of Humanitarian Affairs. “Nigeria Humanitarian Needs Overview 2022 (February 2022) - Nigeria | ReliefWeb,” February 9, 2022.
80 Brechenmacher, Saskia. “Stabilizing Northeast Nigeria After Boko Haram.” Carnegie Endowment for International Peace. Accessed August 2, 2023.
81 USAID. “Nigeria - Complex Emergency Fact Sheet #3 Fiscal Year (FY) 2023.” June 15, 2023.
82 Chimaobi Ibekwe, Christopher, Nneka Perpetua Oli, and Ignatius Uche Nwankwo. “Prevalence of Herdsmen and Farmers Conflict in Nigeria.” Research Gate, January 2018.
83 Korave, Joseph, Samuel Bawa, Bem Ageda, Aondoaver Ucho, Doris Mwuese Bem-Bura, Anthony Onimisi, Boubacar Dieng, et al. “Internal Displacement; an Impediment to the Successful Implementation of Planned Measles Supplemental Activities in Nigeria, a Case Study of Benue State.” Vaccine, Efforts Towards Measles Elimination in Nigeria: Lesson Learnt and Best Practice of the 2017/2018 Measles Vaccination Campaign, 39 (November 17, 2021): C76–81.
84 Omoleke, Semeeh Akinwale, and Menberu Getachew Tadesse. “A Pilot Study of Routine Immunization Data Quality in Bunza Local Government Area: Causes and Possible Remedies.” The Pan African Medical Journal 27, no. 239 (February 8, 2017).
85 Wigley, Adelle, Josh Lorin, Dan Hogan, C. Edson Utazi, Brittany Hagedorn, Emily Dansereau, Andrew J. Tatem, and Natalia Tejedor-Garavito. “Estimates of the Number and Distribution of Zero-Dose and under-Immunised Children across Remote-Rural, Urban, and Conflict-Affected Settings in Low and Middle-Income Countries.” PLOS Global Public Health 2, no. 10 (October 26, 2022): e0001126.
86 Sato, Ryoko. “Effect of Armed Conflict on Vaccination: Evidence from the Boko Haram Insurgency in Northeastern Nigeria.” Conflict and Health 13, no. 1 (October 29, 2019): 49.
87 Babakura, Binta, Terna Nomhwange, Anne E Jean Baptiste, Onome Dede, Lydia Taiwo, Shehu Abba, Margaret Soyemi, et al. “The Challenges of Insecurity on Implementing Vaccination Campaign and Its Effect on Measles Elimination and Control Efforts: A Case Study of 2017/18 Measles Campaign in Borno State, Nigeria.” Vaccine, Efforts Towards Measles Elimination in Nigeria: Lesson Learnt and Best Practice of the 2017/2018 Measles Vaccination Campaign, 39 (November 17, 2021): C66–75.
88 Nnadi, Chimeremma, Andrew Etsano, Belinda Uba, Chima Ohuabunwo, Musa Melton, Gatei wa Nganda, Lisa Esapa, et al. “Approaches to Vaccination Among Populations in Areas of Conflict.” The Journal of Infectious Diseases 216, no. suppl_1 (July 1, 2017): S368–72.
89 Nkwogu, L., Shuaib, F., Braka, F. et al. Impact of engaging security personnel on access and polio immunization outcomes in security-inaccessible areas in Borno state, Nigeria. BMC Public Health 18 (Suppl 4), 1311 (2018).
90 Sbarra, Alyssa N., Sam Rolfe, Emily Haeuser, Jason Q. Nguyen, Aishatu Adamu, Daniel Adeyinka, Olufemi Ajumobi, et al. “Estimating Vaccine Coverage in Conflict Settings Using Geospatial Methods: A Case Study in Borno State, Nigeria.” Scientific Reports 13 (July 8, 2023): 11085.